| Sebaceous hyperplasia |
Minute, profuse yellow-white papules frequently on forehead, nose, lip, and cheeks |
 |
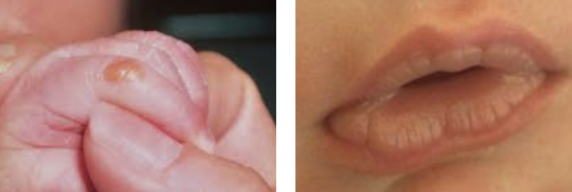
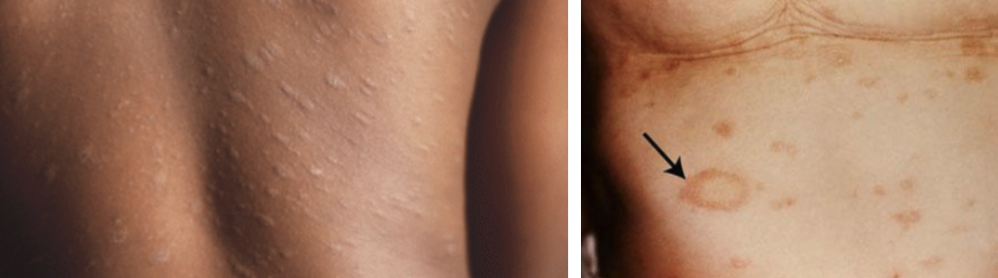
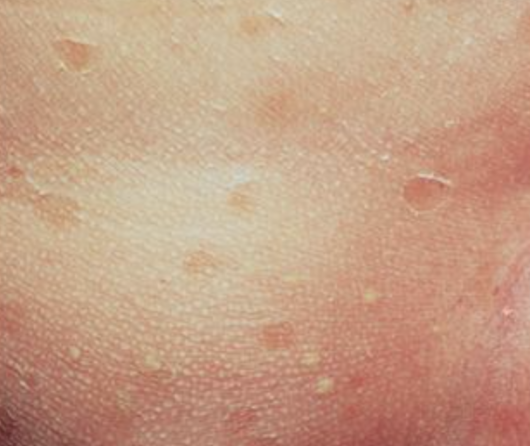
| Milia/miliaria |
1-2 mm pearly, opalescent cysts |
 |
| Neonatal acne (neonatal cephalic pustulosis) |
Inflammatory papules and pustules usually w/o comedonal lesions |
 |
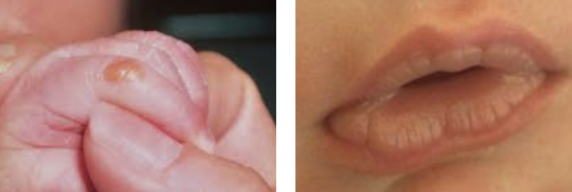
| Sucking blisters |
Solitary or scattered superficial bullae on upper limbs of infants at birth (presumed in utero sucking) |
 |
| Cutis marmorata |
Evanescent, lacy, reticulated red and/or blue cutaneous pattern when exposed to low environmental temperatures |
 |
| Harlequin color change |
When infant (usually immediate newborn period and in low birth weight infants) is laying on side, dependent area is deep red and upper half (longitudinally) is pale |
 |
| Nevus simplex (“salmon patch,” “stork bite,” “angel’s kiss”) |
Small, pink, ill-defined vascular macule usually on glabella, eyelids, upper lip and nuchal area |
 |
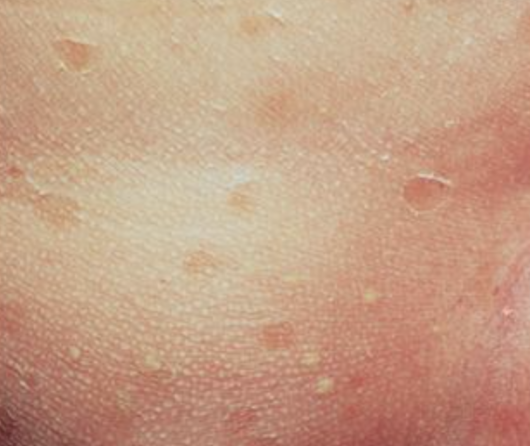
| Erythema toxicum neonatorum (e tox) |
Benign, self-limited evanescent eruption usually in term infants presenting w/ firm, yellow-white papules and pustules w/ a surrounding erythematous flare; palms and soles are almost never affected |
 |
| Transient neonatal pustular melanosis (TNPM) |
Superficial pustules, ruptured pustules w/ a fine scale, and hyperpigmented macules |
 |
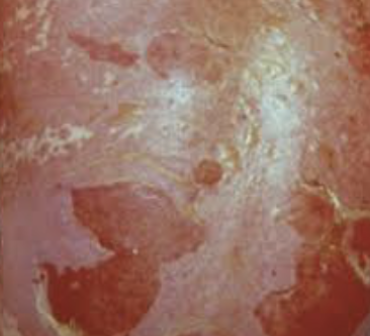
| Seborrheic dermatitis |
Erythema and greasy scales usually on the scalp (“cradle cap”), face, forehead, trunk, intertriginous and flexural areas including diaper |
 |