18 Neonatology (NICU)
18.1 APGAR Scoring
| 0 | 1 | 2 | |
|---|---|---|---|
| HR | <60 | 60-100 | >100 |
| Color | Blue throughout | Pink body & blue extremities | All pink |
| Respiratory effort | No effort | Weak cry, hypoventilation | Strong cry |
| Tone | Limp | Some flexion w/o active movement | Active movement |
| Reflex irritability | No response | Grimace | Cry/cough/sneeze |
18.2 Neonatal Respiratory Disorders & Delivery Room Pathology
- Can be divided into:
- Upper airway blockage (choanal atresia, pharyngeal airway malformation)
- Impaired lung function
18.2.1 Choanal Atresia
18.2.1.1 History
Pink when crying, cyanotic when quiet. Inability to pass NG tube in one or both sides
18.2.1.2 Management
Oral airway, intubation
18.2.2 Pharyngeal Airway Malformation
18.2.2.1 History
Persistent Retractions, poor aeration
18.2.2.2 Management
Prone positioning, posterior nasopharyngeal tube
18.2.3 Congenital Diaphragmatic Hernia (CDH)
18.2.3.1 History
Assymetric lung sounds, cyanosis with bradycardia, scaphoid abdomen.
18.2.3.2 Diagnosis
Most likely on prenatal imaging in patients with prenatal care. Postnatally diagnosed with CXR
18.2.3.3 Management
Intubation, avoid positive pressure! Place orogastric tube.
18.2.4 Pleural Effusion
18.2.4.1 History
Diminished aeration with poor osygenation/ventilation
18.2.4.2 Management
Intubation, needle thoracentesis +/- chest tube. Volume expansion if hemodynamically unstable. Fluid analysis to determine type and source of fluid.
18.2.5 Pneumothorax
18.2.5.1 History
Persistent cyanosis, hypoxemia, +/- bradycardia associated with respiratory distress
18.2.5.2 Diagnosis
CXR
18.2.5.3 Management
Needle thoracentesis immediately, chest tube if recurrent
18.2.6 Meconium Aspiration
18.2.6.1 History
Meconium stained fluid, respiratory distress and/or apnea if severe
18.2.6.2 Diagnosis
CXR
18.2.6.3 Management
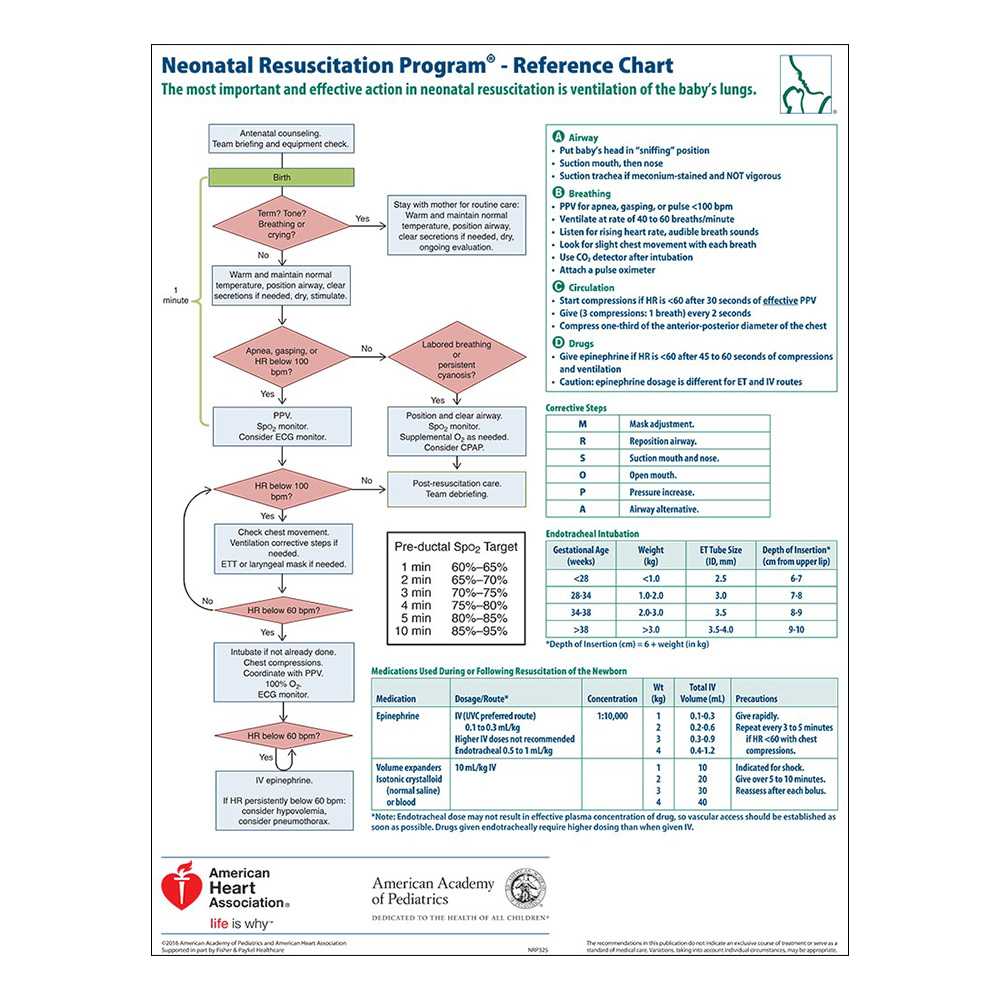
Can deep suction upper airway. Tracheal suctioning not recommended. Intubation per NRP
18.2.6.4 Complications
Can cause lung inflamation and direct surfactant inactivation and one of the causes of persistnet pulmonary hypertension, there is a range of severity but can be quite severe!
18.2.7 Persistent Pulmonay Hypertension (PPHN)
18.2.7.1 History
Asphyxia, mecoumium aspiration, intrinsic lung disease
18.2.7.2 Clinical Manifestations
Hypoxemia, hypotension
18.2.7.3 Diagnostics
CXR with decreased pulmonary vasculature. ECHO with increased R->L shunting.
18.2.7.4 Management
- Ultimate goal is to decrease the pulmonary vascular resistance and increase pulmonary blood flow.
- Oxygenation Index (OI): Helpful numeric index evaluating oxygenation to direct management decisions
- OI = FiO2 x MAP / PaO2
18.2.8 Respiratory Distress Syndrome (RDS)
18.2.8.1 Etiology
Surfactant deficiency, common in premature infants
18.2.8.2 Symtpoms
Hypoxia with respiratory distress
18.2.8.3 Diagnostics
CXR with ground glass opacities, low lung volumes, air bronchograms
18.2.8.4 Management
- CPAP or if severe respiratory distress/apnea intubation
- Surfactant administration if intubated. Can give 2 doses if still intubated 12 hrs after the 1st dose
- Minimize barotrauma and FiO2
18.2.9 Transient Tachypnea of the Newborn (TTN)
18.2.9.1 Etiology
Delayed retention of amniotic fluid
18.2.9.2 History
Typically a term infant, higher risk with birth by C-section.
18.2.9.3 Clinical Manifestations
Tachypnea, respiratory distress, +/- hypoxemia
18.2.9.4 Diagnosis
CXR with prominent vasculature and fluid in the fissures
18.2.9.5 Management
Supportive care, usually improves in 4-6 hrs. If O2 needs or symptoms last longer than 24 hrs, question diagnosis.
18.3 Neonatal Cardiology
NOTE: See Cardiology chapter for full details.
18.3.1 Blood Pressure for Premature Infants
- Can be controversial as there are no normatives in the literature, but rough rule of thumb:
- First 1-2 DOL, MAP = GA (i.e. 24wk infant → goal MAP >24)
- Some evidence that MAP should be > 30 mmHG even for ELBW
- After first few DOL, goal MAP = GA + 5
- For infants w/ PPHN, goal MAP should be based on pulmonary blood flow and urine output, even if it requires higher MAPs than typical for GA (sometimes 40-50 mm Hg)
- First 1-2 DOL, MAP = GA (i.e. 24wk infant → goal MAP >24)
- Key is to monitor urine output, pulses, perfusion, trends in BUN/Cr
18.3.2 Patent Ductus Arteriosus (PDA)
18.3.2.1 Etiology
Failure of ductal tissue to close in the premature infant. Affects about 60% of infants <28 weeks.
18.3.2.2 Clinical Manifestations
- Continuous machine-like murmur
- Hypotension, widened pulse pressure, hyperactive precorium
- Worsening oxygenation and ventilation, secondary to pulmonary over-circulation
- Metabolic acidosis
18.3.2.3 Diagnosis
Echocardiogram
18.3.2.4 Management
- Medical therapy: Indomethacin or ibuprofen or tylenol
- Generally contraindicated if large IVH, severe oliguria, or NEC
- Surgical ligation
- Watch & wait: w/ symptomatic support (i.e. ventilator management, pressors for MAP support)
18.4 Neonatal Hematology
18.4.1 Anemia
18.4.1.1 Definition
Depends on gestation and chronologic age
18.4.1.2 Differential
- Iatrogenic: Frequent blood draws, surgical/procedural blood loss
- Hemorrhagic: Placental abruption, umblical cord disruption at delivery, head trauma (subcaleal, cephalohematoma), NEC, twin-twin transfusion, IVH
- Hemolytic: Rh incompatability, ABO incompatability
18.4.1.3 Work-up
- CBC, retic, type and Coombs, smear, bilirubin, HUS or head imaging if risk for IVH
- At birth: Delivery history, PE, Kleinhauer-Betke on mother (determines if fetal blood is in maternal circulation) in addition to above
18.4.1.4 Management
- NOTE: Transfusion criteria for term and premature infants does not have robust data and is controversial. It tends to be facility dependent.
- Preterm:
- If intubated and acutely ill, Hct 35-40
- If “feeding and growing,” Hct >30 w/ good reticulocyte
- Term:
- If acultely ill, consider transfusing to goal Hct >40
- If hemodynamically stable, goal Hct >25
18.4.2 Polycythemia
18.4.2.1 Definition
Hct >65
18.4.2.2 Differential
Increased fetal production, placental insufficiency, thyrotoxicosis, gestational diabetes (GDM), genetic disorders (e.g. Trisomy 21, Beckwith-Wiedemann), hypertransfusion, delayed cord clamping, twin-twin transfusion
18.4.2.3 Work-up
- CBC, monitor for hypoglycemia, follow bili & electrolytes
- Monitor especially if there are neurologic symptoms or respiratory distress
18.4.2.4 Management
Partial exchange transfusion w/ normal saline, ideally w/ UVC
- Indications: Hct >65 w/ symptoms, >70 and asymptomatic
18.4.3 Thrombocytopenia
18.4.3.1 Definition
Plt <150
18.4.3.2 Differential
- Increased destruction/consumption: Autoimmune, alloimmune (NAIT), infection/DIC/NEC, drug-induced/toxicity, hypersplenism, Kasabach-Merrit Syndrome, following transfusion
- Decreased production: Thrombocytopenia-absent radius, Fanconi anemia, Trisomy 13, 18, 21
- Miscellaneous: Asphyxia, pre-eclampsia, Type 2B Von-Willebrand
18.4.3.3 Work-up
- Labs: Repeat platelet count, coagulation studies
- Imaging: Consider HUS
- Exam for evidence of bleeding
- Maternal history including maternal platelet count
18.4.3.4 Management
Depends on etiology, symptoms, and upcoming needs (i.e. procedures)
- Platelet goals:
| GA | Symptomatic | Asymptomatic |
|---|---|---|
| Term | >50-100k | >20-30k |
| Pre-Term | >100k | >50k |
- Management specific to Neonatal Alloimmune Thrombocytopenia (NAIT):
- Goal plts >20-30k if no active bleeding (use antigen negative platelets to transfuse)
- Check HUS
- Consider steroids or IVIG
- Maternal platelet typing
18.5 Neonatal Neurology
18.5.1 Interventricular Hemorrhage (IVH)
18.5.1.1 Pathophygiolosy
Blood vessel/blood brain barrier development is premature leaving very delicate, fragile blood networks
18.5.1.2 Screening
- Screening criteria (indications for HUS): GA <32 wks, BW <1500g, low Hct, low plts, unstable BPs, prolonged hypotension, cardiopulmonary arrest, pneumothorax, asphyxia, pre/during ECMO
- Timing: DOL 3, 7-10, 30, 60 (consider in first 24 HOL if very ill ELBW)
18.5.1.3 IVH Grading
- Grade I: Germinal matrix hemorrhage (GMH)
- Grade II: Intraventricular hemorrhage without ventricular dilation
- Grade III: Intraventricular hemorrage with ventricular dilation
- Grade IV: Grade III + parenchymal hemorrhage
18.5.2 Therapeutic Cooling
18.5.2.1 BWH Protocol
NOTE: Protocols are site-specific! This section reviews the BWH protocol. Access BMC info via the BMC Infonet.
- Standard eligibility criteria:
- > 34 wks gestation
- Any one of the following:
- Sentinel event prior to delivery
- Apgar score < 5 at 10 min
- Requires PPV, intubation, or CPR at 10 min
- pH < 7.1 from cord or blood gas within 60 min of birth
- Abmormal base excess < -10 meq/L from cord or blood gas within 60 min of birth
- Any one of the following:
- Neonatal encephalopathy score > 4
- Seizure or clinical concern for seizure
- Exclusion criteria:
- Absolute contraindication: <34 wks gestation
- Relative contraindications: Severe IUGR, <1750g, severe congenital anomalies/genetic syndromes/known metabolic disorders, major intracranial hemorrhage, overwhelming sepsis, uncorrectable clinically significant coagulopathy
18.5.2.2 Management
Site-specific as encompassed in respective protocols, but below are some general guides:
- Cardiovascular monitoring
- Total fluid goal of 60 ml/kg/day. Can do up to 10 mL/kg/day of eneteral feeding if clinically stable.
- At BWH, infant will be on starter PN and then custom PN while cooled
- Sedation: Morphine 0.05 mg/kg loading dose, followed by 0.01 mg/kg/hr infusion. Can decrease to 0.005 mg/kg/hr after 12 hrs.
- Neuromonitoring
- EEG for 24 hrs, can be switched to aEEG if EEG w/o seizures
- HUS on admission
- MRI on DOL 4 after re-warming, and after DOL 10-21
- If leaving protocol early, consider MRI 24-48 hrs after rewarming
- Seizures
- Drug of choice: Phenobarbital 20 mg/kg loading dose, w/ serum level 2-12 hrs
- 2nd choice: Fosphenytoin 20 mg/kg
- 3rd choice: Midazolam 0.05 mg/kg IV one time followed by 0.15 mg/kg/hr for 12 hours then taper over 24 hrs
- Lab monitoring (suggested)
- On admission: Lactate, blood gas, CBC, PT/PTT/INR, fibrinogen, blood culture
- At 12 hrs: BMP, Mg, ALT, AST
18.6 Neonatal Infectious Disease
18.6.1 Sepsis
- Use Kaiser Early Onset Sepsis (EOS) risk calculator for > 34 wks
- Otherwise, use clinical illness in coordination w/ maternal fever, ROM, GBS status to help determine treatment
18.6.2 TORCH infections
- When to be concerned: IUGR/SGA (<10th% for age), failed hearing screen, blueberry muffin rash, hepatosplenomegaly, unexplained direct hyperbilirubinemia
- Infections and how to diagnose them:
- Toxoplasmosis: Newborn Screen (NBS)
- Syphilis (other): Maternal screen
- Rubella: Maternal screen
- CMV: Urine CMV shell or Buccal CMV PCR
- HSV: Maternal history or PCR/cultures from suspected lesions on baby. HSV PCR from blood/CSF.
18.6.3 Vertical Transmission
18.6.3.1 Hep B
See Newborn Nursery chapter
18.6.3.2 HIV
Call ID consult w/ maternal labs and history to initiate treatment AS SOON AS POSSIBLE!
18.7 Neonatal Endocrinology
18.7.1 Hypoglycemia
18.7.1.1 Definition
Goal glucose value depends on age:
- 0-4 hours of life (HOL) = >40
- 4-24 HOL = >45
- 24-48 HOL = >50
- Greater than 48 HOL = >60
18.7.1.2 Risk factors
Infant of diabetic mother (IDM), birth weight <2500g, SGA (<10%ile) or LGA (>90%ile), preterm (<37w) or post-dates (>42w), 5-min Apgar <7, maternal meds (beta blocker, terbutaline given to mom w/i 48 hrs of delivery, respiratory distress > 1hr, family history of hypoglycemia, congenital syndrome or midline abnormalities
18.7.1.3 Management
Depends on age and value:
- If mild for age, can feed
- If severe for age, consider D10W 2 mL/kg bolus and/or maintenance D10W at 60 mL/kg/day
18.8 Neonatal Gastroenterology
18.8.1 Emesis in an Infant
18.8.1.1 Differential
Medical vs. Surgical
| Medical | Surgical |
|---|---|
| - Anxiety, excitement - Celiac disease - CAH - Improper feeding - Inborn errors of metabolism - Infection (sepsis, UTI, meningitis) - Esophageal dysmotility - Excessive crying - Food allergies - Gastroenteritis - GERD - Ingestion of maternal blood/mucous - Kernicterus - Milk protein allergy - NEC - Overfeeding |
Annular pacreas - Appendicitis - Atresia, stenosis, webbing - Duplications - Esophageal atresia - Functional ileus - Hernias - Intussusception - Malrotation w midgut volvulus - Meconium ileus - Meconium plug syndrome - NEC w/ perforation - Pyloric stenosis - Testicular torsion - Tracheoesophageal fistula (TEF) - Tumors - Ulcers - Vascular rings |
Bilious vs. Non-Bilious
| Bilious OR Non-Bilious | Likely NON-Bilious |
|---|---|
| - Intestinal atresia - NEC - Meconium plug - Meconium ileus - Malrotation - Volvulus - Hirschsprung Disease |
- Pyloric stenosis - Intussusception - Reflux |
18.8.1.2 Work-up
- Imaging: Always start w/ KUB!
- Ultrasound for anatomic, NEC or intussusception
- Consider contrast study
- Upper if concern for malro/volvulus
- Lower in concern for jejunal/ileal atresia
- Sepsis eval if concerned for NEC
- Bowel rest
- If concerned for surgical diagnosis, consult Surgery
- Further lab evaluation depending on clinical presentation/suspected etiology: CBCd, chem10, blood gas, lactic acid, LFTs, amylase/lipase, BCx, UA/UCx, stool guaiac, consider metabolic/endocrine work-up
18.8.2 Acute Abdomen in the Neonate
| “High” Obstruction | “Low” Obstruction | “Acquired” Disease |
|---|---|---|
| - Esophageal atresia - Duodenal atriesia - Duodenal web - Annular pancreas - Malrotation - Jejunal atresia |
- Ileal atresia - Meconium ileus - Meconium plug - Hirchsprung disease - Anal atresia |
- NEC - Hypertrophic pyloric stenosis - Incarcerated inguinal hernia - Gastroenteritis - Sepsis - Perforated stress ulcer |
| Main symptom: Emesis | Main symptom: Constipation | |
| KUB: No distal bowel gas | KUB: Dilated small bowel loops (proximal to obstruction) and microcolon (distal to obstruction) |
18.8.3 Indirect Hyperbilirubinemia
- ALL infants: Juandice in the first 24 HOL should ALWAYS be considered pathologic and prompt an immediate serum bilirubin, both total and direct
- Infants > 35 wks GA: Use BiliTool
- Premature infants have light level (LL) and exchange transfusion levels based on gestational age (use corrected GA):
| Gestational Age (corrected) | Phototherapy at TsB | Exchange Transfusion at TsB |
|---|---|---|
| <28w 0/7 | 5 | 11 |
| 28w 0/7 to 29w 6/7 | 6 | 12 |
| 30w 0/7 to 31w 6/7 | 8 | 13 |
| 32w 0/7 to 33w 6/7 | 10 | 15 |
| 34w 0/7 to 34w 6/7 | 12 | 17 |
- Other management if approaching exchange transfusion:
- Aggressive phototherapy
- Aggressive hydration (IV + PO)
- IVIG if Coombs positive
- Consider steroids
- Prepare for exchange transfusion (call blood bank)
18.8.4 Neonatal Entercolitis (NEC)
18.8.4.1 Etiology
- Precise etiology unclear
- Affects 10% of premature infants, w/ increased incidence at lower gestational age
- Risk factors: Prematurity, IUGR, preinatal asphyxia, PDA, shock/hypotension, umbilical arterial catheter (UAC), congenital heart disease
18.8.4.2 Clinical Manifestations
- Abdominal distension/discoloration/redness, feeding intolerance, heme positive stools (may be grossly bloody)
- Non-specific systemic symptoms, including: lethargy, apnea, temperature instability, unexplained acidosis, hyperglycemia, poor perfusion
- Lab abnormalities: Hyponatremia, hyperkalemia, metabolic acidosis, leukocytosis or leukopenia, thrombocytopenia
18.8.4.3 Work-up
- Labs: CBCd, blood culture, electrolytes
- Imaging: KUB w/ left lateral decub
18.8.4.4 Management
- Supportive care
- Place replogle tube for decompression
- Antibiotics, start IVF/TPN
- Monitor labs and KUB serially
- Surgery consult
18.8.5 Malrotation (+/- Mid Gut Volvulus)
18.8.5.1 Etiology
- Developing bowel fails to undergo usual counterclockwise rotation during 4th-10th wk of embryogenesis
- Peritoneal bands that usually attach bowel to central body axis are misplaced and compress duodenum, resulting in partial obstruction
- Volvulus results in intestinal obstruction
- Superior mesenteric artery may be compressed leading to ischemia
18.8.5.2 Clinical Manifestations
- Newborn <1mo w/ bilious emesis
- Associated w/ diaphragmatic hernia, omphalocele, gastroschisis
18.8.5.3 Work-up
- KUB: Usually unremarkable, may have signs of small bowel obstruction
- UGI: Abnormal position of duodenal-jejunal junction. Volvulus appears as spirla corkscrew of duodenum.
- US: May show volvulus in small bowel
18.8.5.4 Management
Emergent surgical intervention
- Modified Ladd’s Procedure:
- Division of peritoneal bands around the duodenum
- Colon placed on the left w/ duodenum on the right, to broaden the mesentery
- Appendectomy preformed so no confusion w/ future abd pain
18.8.6 Duodenal Atresia
18.8.6.1 Etiology
Embryogenic. 1 in 5,000 live births. 25% have Trisomy 21.
18.8.6.2 Clinical Manifestations
Bilious vomiting hours after birth w/o abdominal distention
18.8.6.3 Work-up
KUB shows double bubble sign (gaseous distension of stomach and proximal duodenum)
18.8.6.4 Management
- NPO w/ NG suction
- Surgical consult for duodenoduodenostomy
18.8.7 Jujonoileal Atresia
18.8.7.1 Etiology
- Mesenteric vascular accident during fetal life
- 1 in 3,000 live births
18.8.7.2 Clinical Manifestations
Bilious vomiting hours after birth w/ abdominal distension, failure to pass meconium; hyperbilirubinemia
18.8.7.3 Work-up
KUB shows air-fluid levels
18.8.7.4 Management
- NPO w/ NG suction
- Surgical consult for resection and anastomosis
18.8.8 Meconium ileus
18.8.8.1 Etiology
5% of newborns with cystic fibrosis, and in 1 per 5,000 to 10,000 live births
18.8.8.2 Clinical Manifestations
Abdominal distension and vomiting hours after birth, failure to pass meconium
18.8.8.3 Work-up
- KUB shows distension, air fluid levels
- Contrast enema shows microcolon +/- inpacted meconium pellets
18.8.8.4 Management
- NPO w/ NG suction
- Water soluble contrast enema
- Surgical enterostomy if needed