27 Toxicology
27.1 Key Resources
- Poison Control: 1-800-222-1222
- BCH Toxicology Fellow/Attending (on call 24/7)
- BCH Chemistry Fellow (daytime hours, can help interpret labs and select specialized testing)
- Hazmat Team: Boston Fire Department
- MSDS: Material Safety Data Sheets
- www.maripoisoncenter.com
- www.aapcc.org
27.2 Approach to Poisoned Patient
27.2.1 Stabilization
Airway, Breathing, Circulation, Disability, Drugs/D-Stick, Decontamination
27.2.2 Physical Exam
Vital signs Neuro: MS, tone, clonus, abnormal movements Eyes: pupils, EOM, nystagmus Mouth: corrosive lesions, odors CV: rate, rhythm, perfusion Resp: rate, depth of respirations, air entry, wheeze GI: motility (?bowel sounds), corrosive effects (i.e. vomiting) Skin: color, bullae, burn, sweat, track marks
27.2.3 History
- AMPLE: Allergies, Meds/Toxins (everyone in home), Past medical history, Last meal, Events
- Known toxin: amount, time since ingestion, early sx, home tx
- Concern for poisoning: h/o pica or ingestions, meds in home, recent illnesses, visitors/events
27.2.4 Basic Labs
Consider ABG, co-oximetry, CBC, D-stick, EKG, Chem, LFTs, serum OSM, UA, urine/serum tox
27.2.5 Tox Screens
Substances included, limits of detection vary hospital to hospital
Urine drug screens rarely inform acute management decisions
Urine tox screens: detect amphetamines, MDMA, barbiturates, benzos, cocaine, opioids, +/- THC
- Qualitative (+/-)
- Does not detect synthetic cathinones (i.e. “bath salts”); false + and false - (esp benzos, synthetic opioids) common
- ADHD drugs: adderall → positive amphetamine
Urine THC - must order separately at BMC
Expanded opioid panel, urine (BMC): detects buprenorphine, oxycodone, methadone, fentanyl
Extended tox screen: GC/MS, urine better than serum, send out test
Meconium tox: amphetamines, THC, cocaine, opiates, PCP
Serum tox: APAP, ASA, EtOH (quantitative),TCAs (qualitative) Specific drug levels: can request agents not on tox screens (digoxin, lithium, AEDs, iron, etc.)
27.2.6 Management
- Can I decontaminate?
- Can I enhance the elimination of the toxin? (www.extrip-workgroup.org)
- Is there an antidote?
- How can I provide the best, targeted supportive care?
27.3 Toxidromes
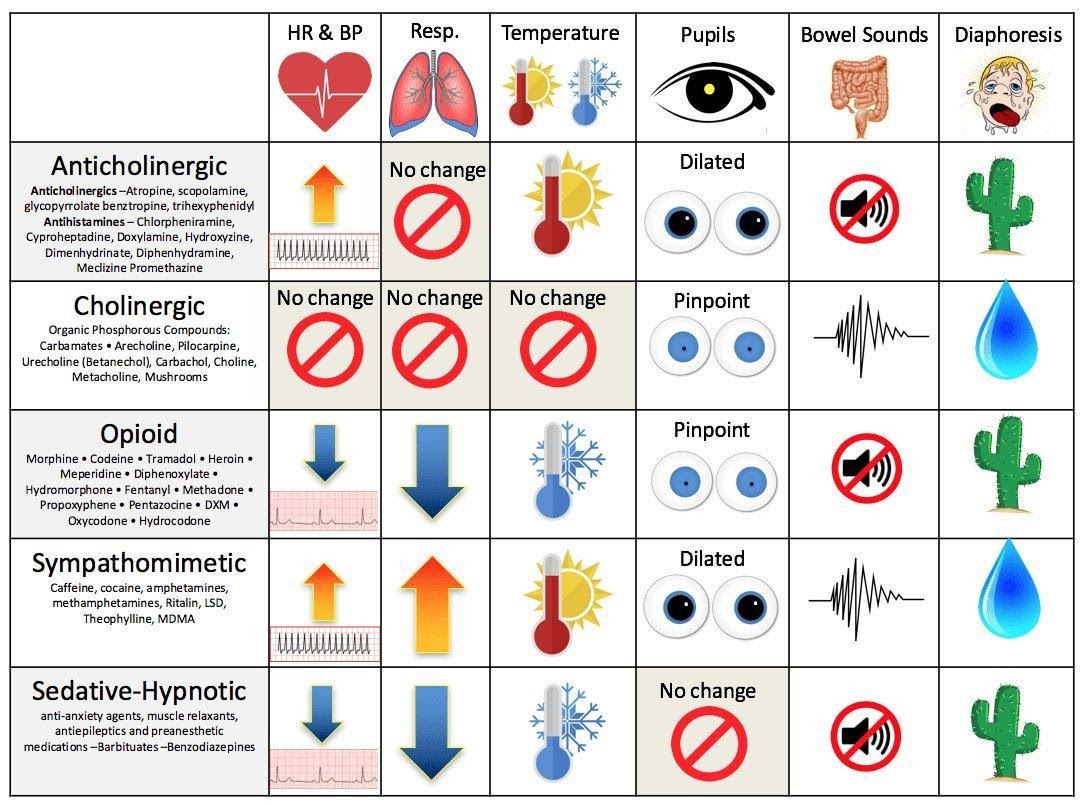
toxidromes_table
27.4 Differential Diagnosis (non-exhaustive)
27.4.1 Temperature
Hyperthermia: NASA - NMS, nicotine - Antihistamines, alcohol withdrawal, anesthetics - Salicylates, sympathomimetics, serotonin syndrome - Anti: -cholinergics, -depressants, -psychotics
Hypothermia: COOLS - Carbon monoxide - Opioids - Oral hypoglycemics - Liquor - Sedative-hypnotics
27.4.2 Heart Rate
Tachycardia: FAST - Free base or other forms of cocaine - Anticholinergics, antihistamines, antipsychotics, amphetamines - Sympathomimetics - Theophylline, TCAs, thyroid hormones
Bradycardia: PACED
- Propranolol (beta-blockers), poppies (opioids), physostigmine
- Anticholinesterase drugs, antiarrhythmics
- Clonidine, calcium channel blockers
- Ethanol or other alcohols
- Digoxin, digitalis
27.4.3 Blood Pressure
Hypertension: CT SCAN - Cocaine - Thyroid supplements - Sympathomimetics - Caffeine - Anticholinergics, amphetamines - Nicotine
Hypotension: CRASH - Clonidine, calcium channel blockers - Rodenticides (containing arsenic, cyanide) - Antidepressants, aminophylline, antihypertensives - Sedative-hypnotics - Heroin (opioids)
27.4.4 Respiratory Rate
Tachypnea: PANT - PCP - Aspirin and other salicylates, acute lung injury (hydrocarbons, vaping) - Noncardiogenic pulmonary edema - Toxin-induced metabolic acidosis
Hypopnea: SLOW - Sedative - hypnotics (benzodiazepines, barbiturates) - Liquor - Opioids - Weed
27.4.5 Blood Glucose
Hyperglycemia: CAPT ABC - Corticosteroids - Antibiotics (quinolones) - Protease inhibitors - Thiazides - Atypical antipsychotics - Beta-agonists - Corticosteroids
Hypoglycemia: HOBBIES - Hypoglycemics (oral) - Other (quinine, unripe ackee fruit) - Beta-blockers - Insulin - Ethanol - Salicylates (late)
27.5 Acetaminophen Overdose
27.5.1 Toxic Dose
200 mg/kg (7.5-10 g in older pts) as a single acute overdose
27.5.2 Pathophysiology
Saturation of glucuronidation/sulfate conjugation pathway → ↑ metabolism via P450 pathway and depletion of glutathione → build up of toxic NAPQI → hepatotoxicity +/- renal toxicity
27.5.3 Symptoms
See chart below
27.5.4 Evaluation
Acetaminophen levels (at ≥ 4 hours post-ingestion, LFTs, coags, electrolytes, BUN/Cr, UA w/ tox screen (serum and urine), urine pregnancy for females
27.5.5 Management
Activated charcoal if w/i 1-2 hrs of ingestion and no contraindications (unprotected airway and decreased LOC)
Goal: Initiate NAC ≤ 8 hours of ingestion (or ASAP if >8 hours post-ingestion)
APAP level → apply NOMOGRAM → estimate risk of hepatotoxicity
KEY POINT: NOMOGRAM can ONLY be used for: single acute ingestion, known time of ingestion, ingestion w/i 24hrs of presentation. Also, caution if coingestants that may affect GI motility
- Risk of hepatotoxicity → give N-acetylcysteine
- IV: loading dose of 150mg/kg over 1 hour, then 50 mg/kg over 4 hours, then 100 mg/kg over 16 hours; check APAP levels, LFTs, coags 2 hours before 16h infusion is scheduled to end
- PO/NG: Loading dose 140mg/kg then 70mg/kg 14hrs x24 hours
- Guidelines for stopping NAC: clinically well, improving LFTs, normalizing coags, APAP level <10 (if patient does not meet guidelines, continue NAC (100mg/kg IV over 16 hours) until they meet criteria.
King’s College Criteria for Liver Transplant:
pH < 7.3 or
INR > 6.5 AND serum creatinine > 3.4mg/dL AND grade III - IV encephalopathy
West Haven Criteria for encephalopathy:
- I: Changes in behavior with minimal change in level of consciousness
- II: Gross disorientation, drowsiness, possible asterixis, behavior changes
- III: Marked confusion, incoherent speech, sleepy but arousable to voice
- IV: Comatose, unresponsive to pain, decorticate/decerebrate positioning
27.5.6 Rule of 150
- Potentially toxic dose: 150mg/kg
- Treatment line: 150mcg/mL at 4 hours
- Loading dose of NAC 150mg/kg over one hour
| A cute APAP To xici ty | Symptoms | Labs |
|---|---|---|
| S tage 1: 0-24 h ours | N/V, diaphoresis, malaise May be asymptomatic | Labs, PE generally normal |
| S tage 2: 2 4-72 h ours | Initial symptoms resolve RUQ pain, liver enlargement/tenderness | AST/ALT, ↑ PT/INR, renal d ysfunction, ↑ amylase |
| S tage 3: 7 2-96 h ours | N/V, diaphoresis return - Jaundice, hepatic encephalopathy, hyperammonemia, bleeding, hypoglycemia, lactic acidosis - Renal failure, multi organ failure, death | LFTs peak |
| S tage 4: 4-14 days | Recovery phase Slow normalization of symptoms and lab values (Symptoms typically normalize well before transaminases do) | Slow no rmalization |
27.6 Aspirin Overdose
27.6.1 Toxic Dose
150 mg/kg
27.6.2 Pathophysiology
- Stimulates medullary respiratory center → ↑RR, hyperpnea, respiratory alkalosis
- Inhibits Kreb’s cycle enzymes → lactic acidosis, ketoacidosis
- Inhibits platelet function + vitamin-K dependent clotting factors → coagulopathy
27.6.3 Symptoms
- Mild toxicity: GI upset, tinnitus and tachypnea
- Moderate toxicity: fever, diaphoresis, tachycardia, agitation, confusion
- Severe toxicity: coma, pulmonary edema, seizures
27.6.4 Evaluation
Serum salicylate level (normal <30 mg/dL), ABG (primary respiratory alkalosis, primary anion-gap met acidosis), glucose (elevated - early, low - late), Electrolytes (hyper/hyponatremia, hypokalemia) +/- LFTs, CBC, coags, UA, serum/urine tox screen. Resulting acidosis and electrolyte changes MAY demonstrate EKG changes (ex. widened QRS, AV block, arrhythmias)
27.6.5 Management
- GI decontamination: activated charcoal (consider repeat dose, prone to bezoar formation)
- Aggressive fluid resuscitation (lots of insensible losses)
- Urine alkalinization: goal URINE pH = 8, goal SERUM pH 7.45-7.55 to enhance ion trapping; can use D5 W150 mEq/L Na-bicarb
- Potassium repletion
- Follow salicylate levels q1-2 hours
- Hemodialysis (ASA level >90-100mg/dL (acute overdose), >60 mg/dL (chronic overdose), severe acidosis or electrolyte disturbances, renal failure, pulm edema, neurologic symptoms, deterioration despite interventions)
27.7 Beta-Blocker Overdose
27.7.1 Toxic Dose
“One pill can kill” in toddlers
27.7.2 Pathophysiology
adrenergic antagonist → ↓ sympathetic outflow
27.7.3 Symptoms
Bradycardia, hypotension, bronchospasm, coma, seizures, hypoglycemia
27.7.4 Evaluation
DS (hypoglycemia), EKG (brady, AV block, accelerated junctional rhythm), serum/urine tox (in cases of suspected intentional ingestions)
27.7.5 Management
- GI decontamination: activated charcoal (consider whole bowel irrigation) if indicated and no contraindications
- Glucagon bolus: 0.15 mg/kg then infusion of 0.05-0.1 mg/kg/hr (for symptomatic bradycardia)
- Fluids +/- pressors for hypotension
- Hyperinsulinemia/euglycemia (HIE) therapy: sometimes used in severe BB OD
27.8 Calcium Channel Blocker Overdose
27.8.1 Toxic Dose
“One pill can kill” in toddlers; individual drug selectivity for cardioactive vs vasoactive effects lost in significant overdose
27.8.2 Pathophysiology
Block L-type Ca channel blockers (affect myocyte contractility, SA nodal AP initiation)
27.8.3 Symptoms
Bradycardia, hypotension, coma, seizures, dihydropyridine CCBs (amlodipine, nifedipine, etc) can present w/ TACHYcardia and relative hypotension, HYPERglycemia
27.8.4 Evaluation
DS (hyperglycemia), EKG (bradycardia, AV block, accelerated junctional rhythm, wide QRS, ST changes), serum/urine tox (in cases of suspected intentional ingestions)
27.8.5 Management
- GI decontamination: activated charcoal (consider whole bowel irrigation) if indicated and no contraindications
- IV calcium chloride or calcium gluconate
- HIE (hyperinsulinemia/euglycemia) therapy: 1 unit/kg bolus of regular insulin then 0.5-1+unit/kg/hr infusion
- Intralipid 20%: 1.5ml/kg during 2-3 mins, followed by 0.25 ml/kg/min IV x 30-60 min (consult Tox)
27.9 Antidepressants: SSRIs and SNRIs
27.9.1 Toxicity
- SSRIs: less toxic than MAOIs or TCAs; most fatalities due to co-ingestion
- SNRIs: greater toxicity than SSRIs (but less than MAOIs or TCAs)
27.9.2 Pathophysiology
Inhibit serotonin +/- norepinephrine reuptake (primarily in CNS)
27.9.3 Symptoms
- Vomiting, CNS depression, tachycardia
- Serotonin syndrome: altered mental status, neuromuscular hyperexcitability (clonus, rigidity, hyperreflexia), autonomic instability (hyperthermia, tachy, HTN) → can lead to rhabdo, seizures, renal failure, DIC
27.9.4 Evaluation
Electrolytes, serum/tox screen, EKG (↑QTc, rare ↑ QRS w/ some SNRIs); levels not helpful
27.9.5 Management
- Decontamination and supportive care
- Benzos and/or serotonin antagonists (cyproheptadine) for serotonin syndrome, consider cooling and paralysis for severe serotonin syndrome
27.10 Antidepressants: TCAs
27.10.1 Toxic Dose
“One pill can kill” in toddlers
27.10.2 Pathophysiology
Peripheral and central anticholinergic, peripheral alpha-1 adrenergic blockade, inhibits CNS NE and serotonin reuptake, blocks cardiac fast Na channels, blocks GABA receptors
27.10.3 Symptoms
- Anticholinergic toxidrome (see toxidrome chart)
- Neurotoxicity (seizures, coma)
- Cardiovascular toxicity (arrhythmias, refractory hypotension, widened QRS)
27.10.4 Evaluation
Electrolytes, CK, D-stick, urinalysis, tox screens, TCA level not useful (other than to confirm ingestion), EKG (prolonged QRS (>100ms a/w seizure, dysrhythmias), sinus tach, vent arrhythmias, lead aVR prominent R waves)
27.10.5 Management
- Gastric decontamination, close monitoring, EKGs
- NaHCO3 titrated to serum pH 7.45-7.55 (indicated for QRS > 100ms w/ other signs of TCA toxicity, vent. arrhythmias, CV collapse, seizures). Mechanism: increase pH -> increase non-ionized TCA = cannot bind sodium channels. Also increases gradient across cardiac cell membranes -> attenuates TCA-induced blockade of rapid sodium channels.
- Supportive care (treat refractory hypotension w/ alpha-agonist pressors)
- For severe TCA overdoses, consider intralipid
27.11 Antidepressants: Buproprion
27.11.1 Toxic Dose
“One pill can kill” in toddlers
27.11.2 Pathophysiology
Dopamine and NE reuptake inhibitor w/ some serotonin reuptake blockade; contraindicated in eating disorder patients given ↑ seizures
27.11.3 Symptoms
Seizures, agitation, HTN, tachycardia, arrhythmias
27.11.4 Evaluation
Levels not helpful, electrolytes, EKG (QRS and QTc prolongation). May cause +amphetamine screen
27.11.5 Management
Supportive care, benzos for seizures, admit for >24 hours to monitor for late onset seizures if ingested Wellbutrin SR, ↑ QRS treated w/ IV sodium bicarb (though may not be as effective)
27.12 Iron
27.12.1 Toxic Dose
- Less than 20mg/kg elemental iron usually asymptomatic
- 20-60 mg/kg: variable response
- Greater than 60 mg/kg: greatest risk of serious toxicity (death reported at 60-300+ mg/kg)
27.12.2 Pathophysiology
Direct caustic effect on GI mucosa → hemorrhagic necrosis; multisystem toxicity 2/2 mitochondrial poison; iron absorbed at duodenum/jejunum
27.12.3 Symptoms
If no significant GI symptoms w/i first 6 hrs after overdose, very low likelihood of significant toxicity
|
GI sx: vomiting, diarrhea, GI bleeding |
|---|---|
|
Latent period: apparent improvement |
|
Hepatotoxicity: hepatocellular injury, AG metabolic acidosis (↑ lactic acid), coma, seizures, multi-organ failure, shock Labs: ↑ bili, ↑ LFTs, ↑ glucose, ↑ PT/INR, ↑ BUN |
|
Late effects: possible bowel obstruction secondary to strictures |
27.12.4 Evaluation
KUB (radio-opaque pills), Fe level, VBG/ABG, lytes, BUN/Cr, glucose, LFTs, PT/INR, CK
27.12.5 Management
Support ABC’s, replace fluid/blood losses, GI decontamination, IV deferoxamine (severe sx, iron level > 500 mcg/d w/ clinical symptoms, sig AG met acidosis)
27.13 Lead
27.13.1 Toxic Dose
No safe lead level exists
27.13.2 Pathophysiology
Interferes w/ interactions of divalent cations and sulfhydryl groups leading to widespread physiologic effects and clinical toxicity
27.13.3 Symptoms
- Lower levels: Abdominal pain, constipation, anorexia, vomiting, developmental delays, aggression, hyperactivity
- Higher levels: drowsiness, clumsiness, ataxia
- Severe levels: decreased consciousness, coma, seizures, death (usually 2/2 cerebral edema)
27.13.4 Evaluation
Lead levels, CBC (microcytic anemia + basophilic stippling of RBC), FEP (free erythrocyte protoporphyrin), BUN/Cr, AST/ALT, x-ray (radiopaque flecks)
27.13.5 Management
- CDC Child Lead Poisoning Program: https://www.cdc.gov/nceh/lead/default.htm
- See also BCH lead poisoning EBG
- Prevention is key: screening and lead levels at WCC (9-12 mo, 2 years)
- Gastric decontamination: whole bowel irrigation
- Chelation therapy (depending on lead levels)
- Seminal Article: CDC. Managing elevated blood lead levels among young children: Recommendations from the Advisory Committee on Childhood Lead Poisoning Prevention, Atlanta: CDC; 2002
- BCH has a separate Environmental Health clinic and service that can assist w/ management
27.14 Drugs of Abuse
27.14.1 Ethanol
27.14.1.1 Hx/PE
Euphoria, loss of coordination, ataxia, slurred speech, nystagmus, nausea, vomiting, hypoglycemia (especially in young children), seizures, coma, respiratory depression
27.14.1.2 Dx
Blood ethanol level, D-stick
27.14.1.3 Management
Supportive; secure airway if unresponsive, no gag reflex
27.14.2 Marijuana
27.14.2.1 Hx/PE
Pupils unchanged, injected conjunctiva, tachycardia, increased appetite, euphoria, anxiety, time-space distortions, panic reaction, psychotic reaction; can cause ataxia and significant sedation in toddlers. Ask about routes of exposure (smoking, vaping, dabbing, edibles, etc.); edibles particularly problematic in young children.
27.14.2.2 Dx
Urine drug screen (note, synthetic cannabinoids not detected on standard urine toxicology screens
27.14.2.3 Management
Supportive care, can treat w/ anxiolytics if needed. Some young children may require airway protection due to degree of sedation.
27.14.3 Stimulants (Amphetamines, Cocaine, Ecstasy/MDMA, “Bath Salts”)
27.14.3.1 Hx/PE
Tachycardia, hyperthermia, mydriasis, diaphoresis, restlessness, tremors, panic, agitations, psychosis, seizures
27.14.3.2 Dx
Urine drug screen; EKG (cocaine may cause QRS widening); troponin if chest pain; CK if concern for rhabdo; electrolytes (hyponatremia w/ MDMA)
27.14.3.3 Management
Supportive care including fluids, avoid beta blockers in HTN due to unrestrained alpha-agonism, benzos for agitation, HTN, and tachycardia
27.14.4 Opioids
27.14.4.1 Hx/PE
Respiratory depression (hallmark), miosis, CNS depression, hypotension, hypothermia, pulmonary edema
27.14.4.2 Dx
Urine drug screen (extended screen available at BMC, typically done as send-out at BCH); EKG (methadone can cause QTc prolongation)
27.14.4.3 Management
Naloxone for severe respiratory/CNS depression, titrate dosing to severity of presentation (may precipitate withdrawal in chronic users); otherwise supportive
27.14.4.4 Notes
Opioids are one of the “one pill can kill” medications in toddlers