2 Rapid Reference
2.1 Calling for Help
BCH
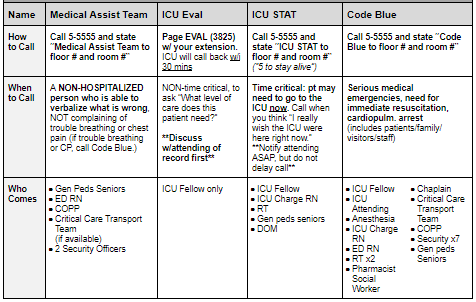
BMC
2.2 PALS
PALS Quick References
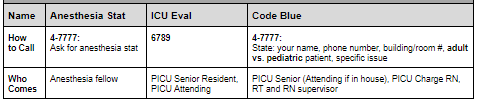
Vital Signs in Children
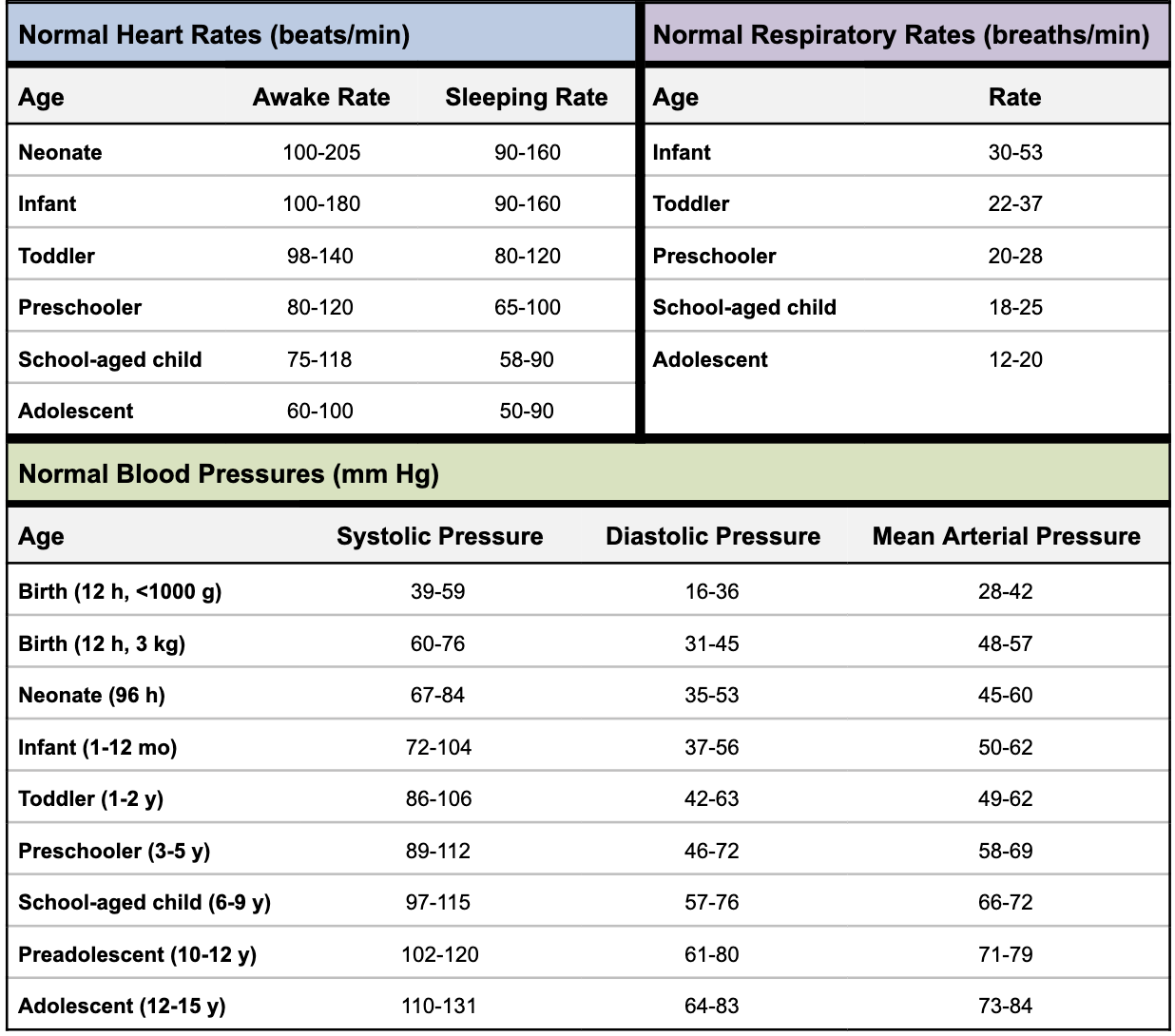
Pediatric Color-Coded Length-Based Resuscitation Tape
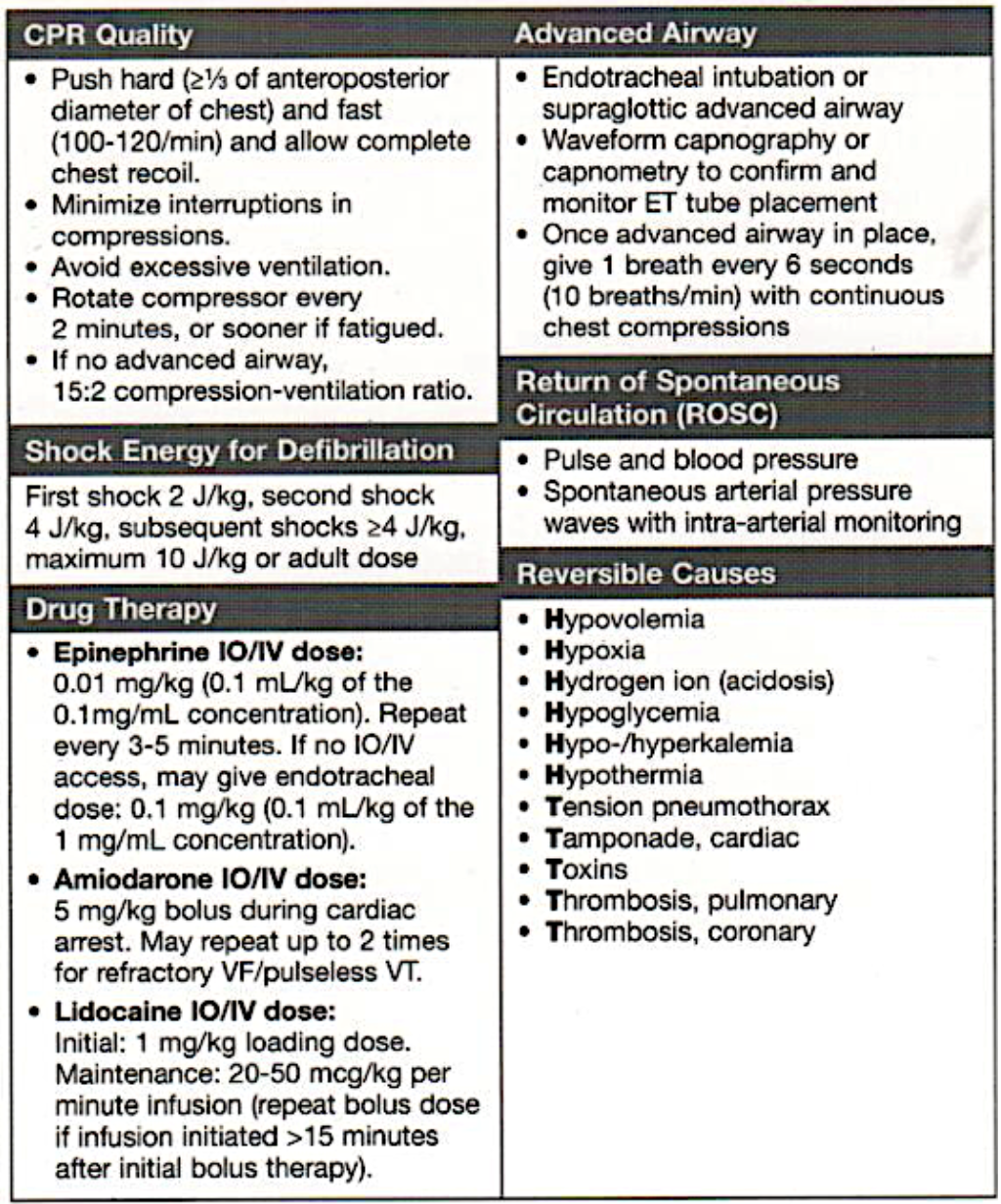
PALS Algorithms
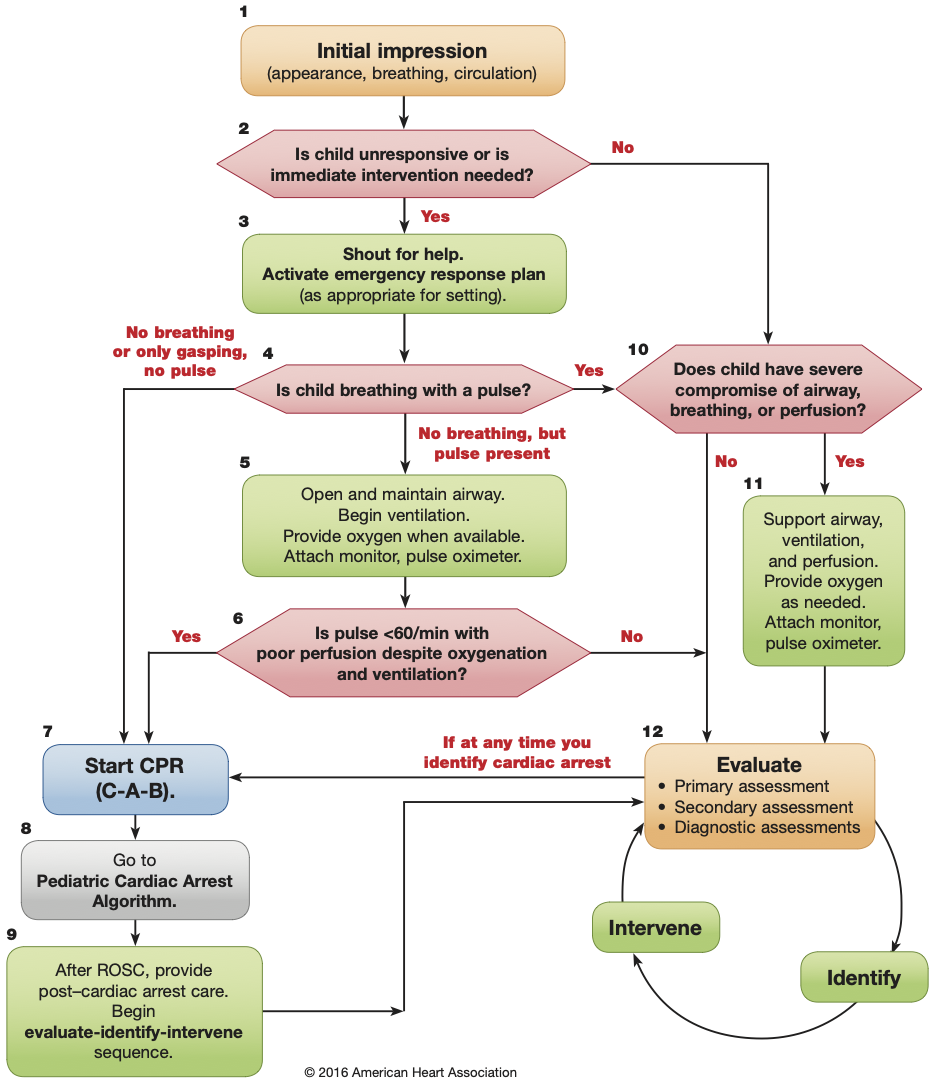
PALS Systematic Approach Algorithm
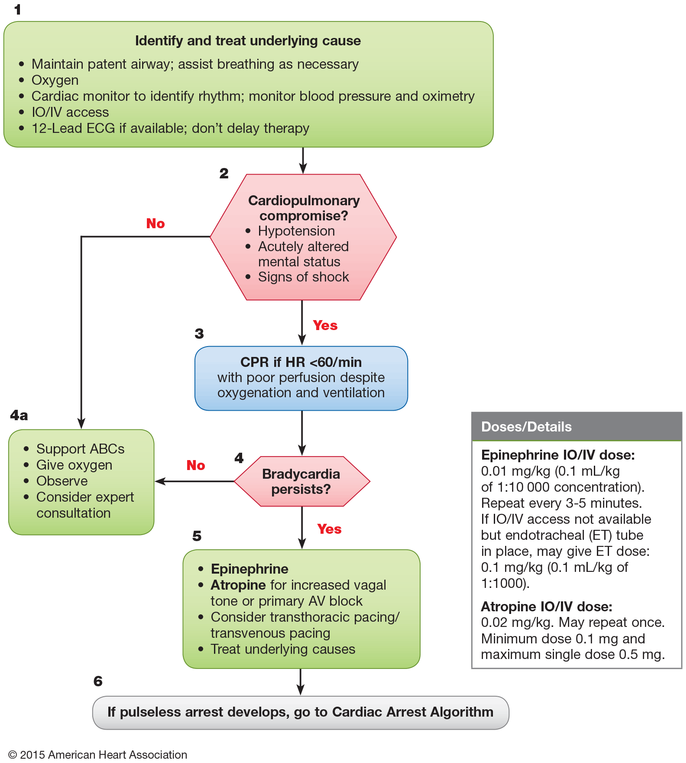
Bradycardia with a Pulse and Poor Perfusion Algorithm
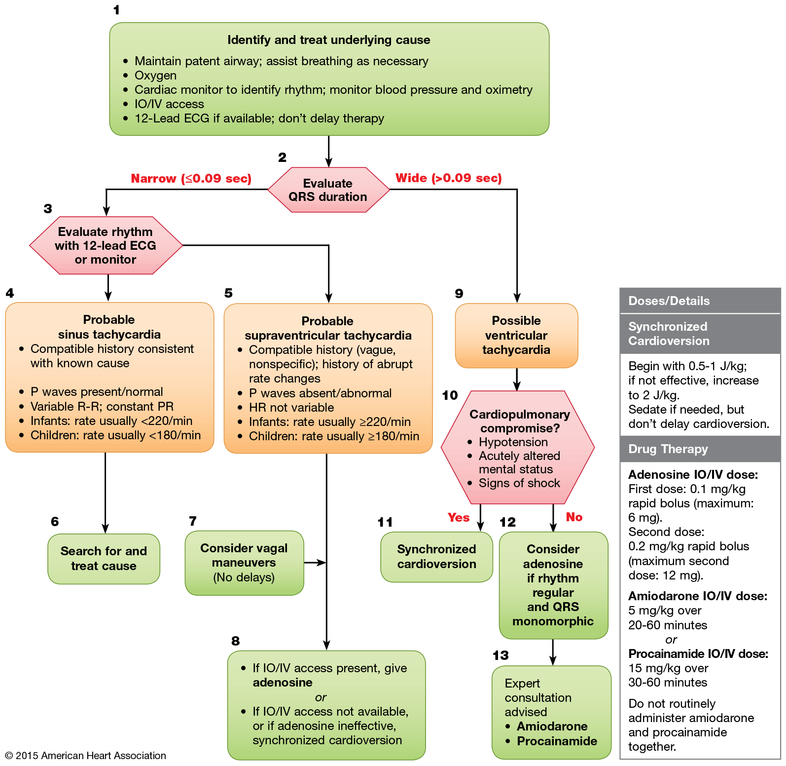
Tachycardia with a Pulse and Poor Perfusion Algorithm
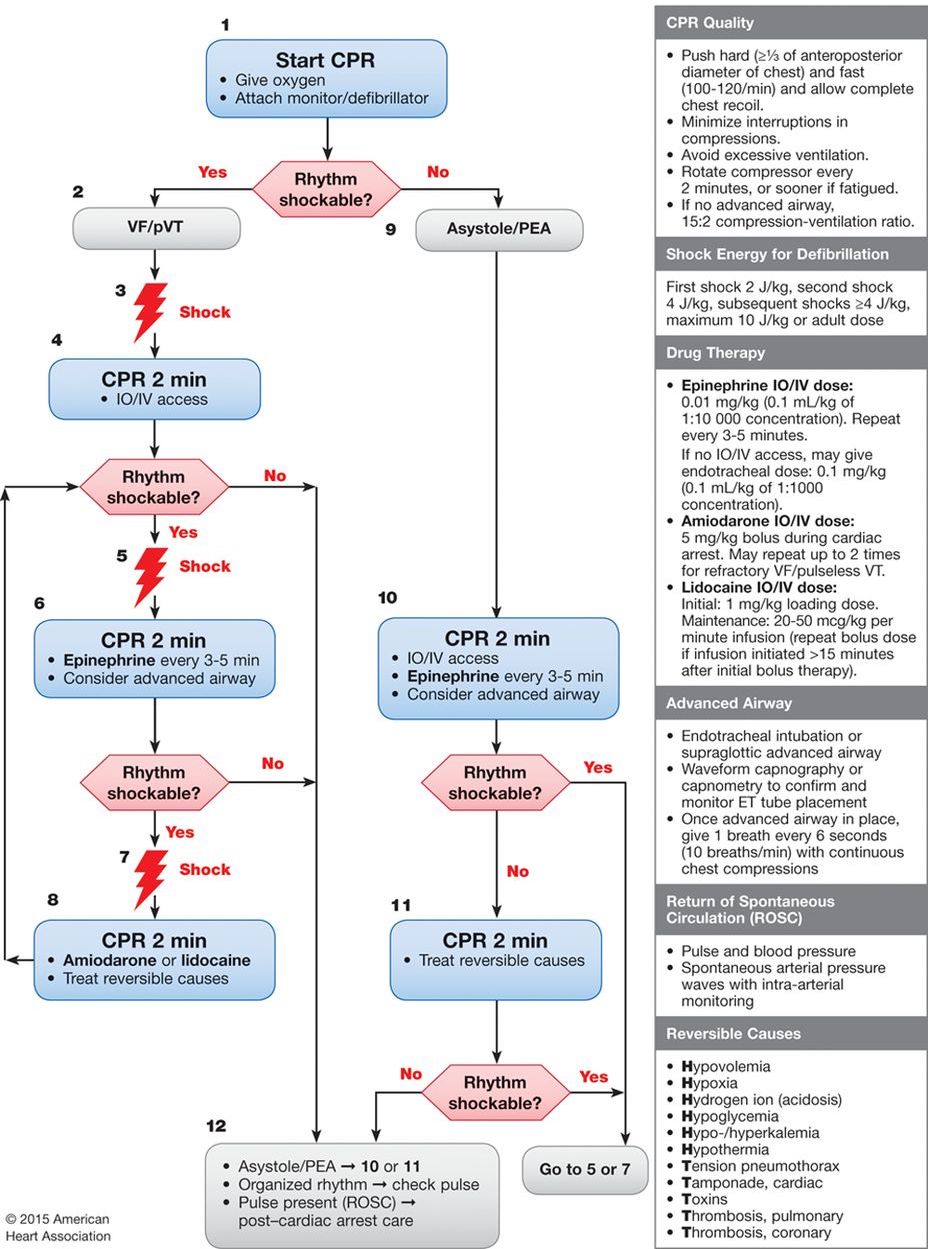
Cardiac Arrest
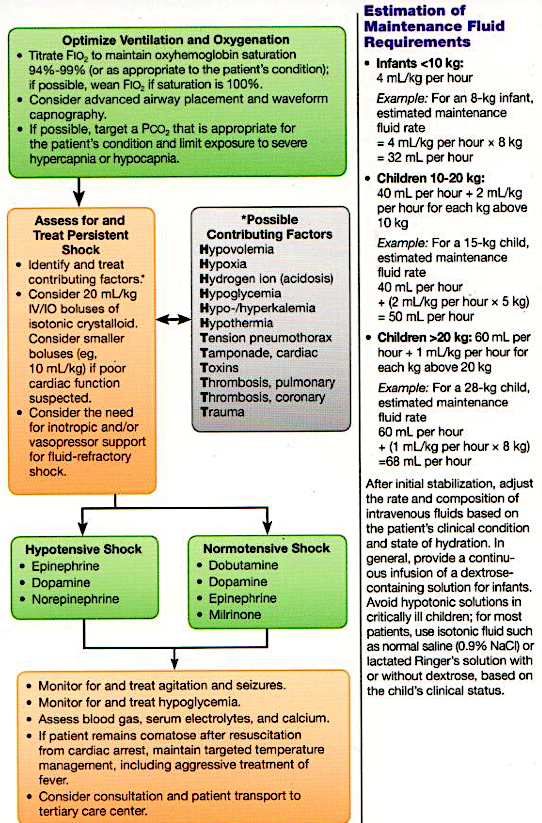
Management of Shock After ROSC Algorithm
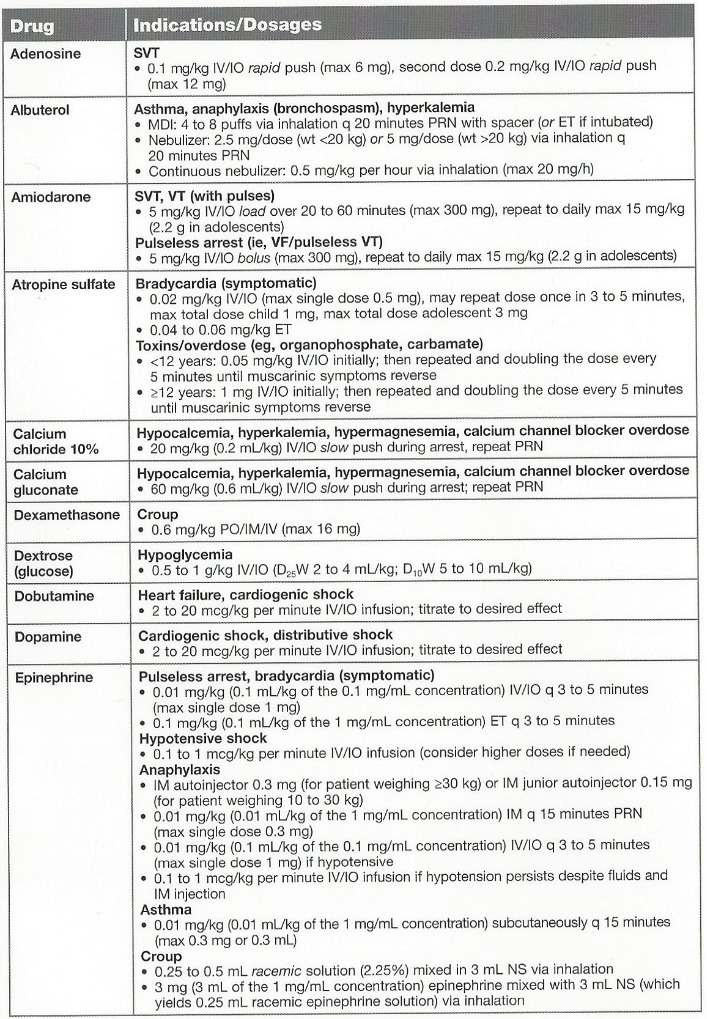
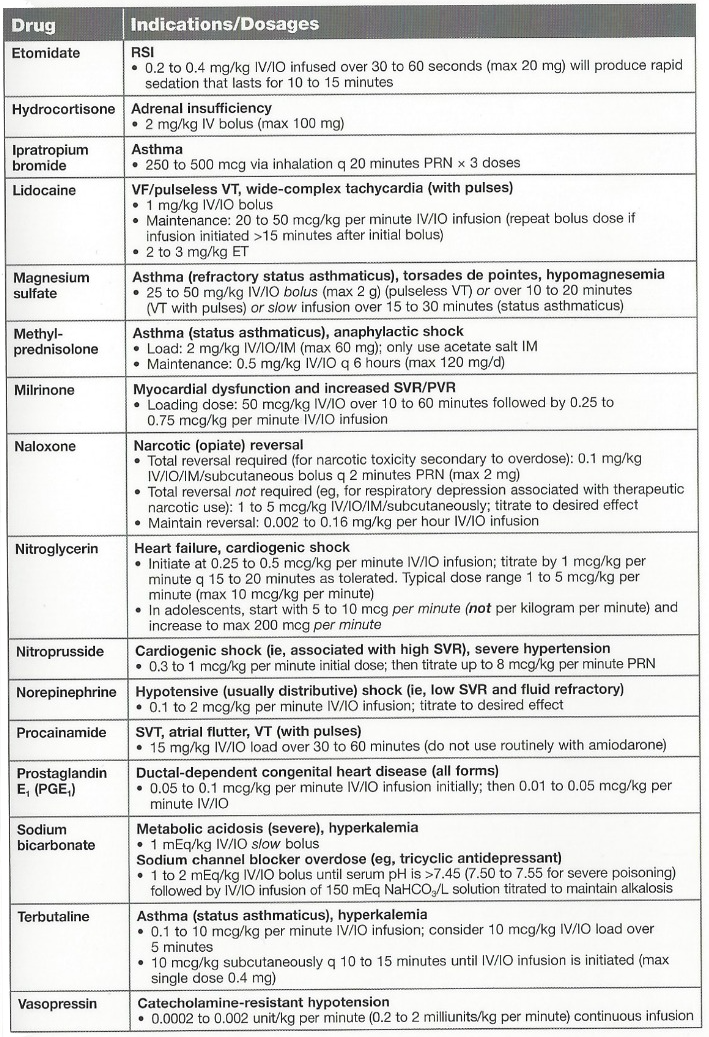
Drugs Used in PALS
2.2.1 Shock
Recognition of Shock
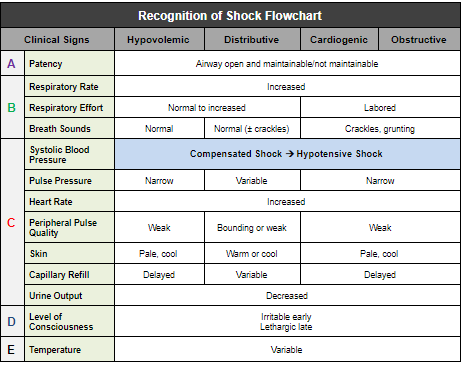
Management of Shock
- Oxygen
- Pulse oximetry
- ECG monitor
- IV/IO access
- BLS as indicated
- POCT glucose
Hypovolemic Shock
| Non-hemorrhagic | Hemorrhagic |
|---|---|
| 20 mL/kg NS/LR bolus, repeat PRN | Control external bleeding |
| Consider colloid NS/LR bolus, repeat 2 or 3x PRN | 20 mL/kg NS/LR bolus, repeat 2 or 3x PRN |
| Transfuse pRBCs PRN |
2.2.1.1 Distributive Shock
Septic
Management Algorithm: Septic Shock
Anaphylactic
IM epinephrine (or autoinjector)
Fluid boluses (20mL/kg NS/LR)
Albuterol
Antihistamines, corticosteroids
Epinephrine infusion
Neurogenic
20mL/kg NS/LR bolus, repeat PRN
Vasopressor
2.2.1.2 Cardiogenic Shock
Bradyarrhythmia/Tachyarrhythmia
Other (e.g. CHD, myocarditis, cardiomyopathy, poisoning)
5 to 10 mL/kg NS/LR bolus, repeat PRN
Vasoactive infusion
Consider expert consultation
2.2.1.3 Obstructive Shock
Ductal-Dependent (LV outflow obstruction)
Prostaglandin E1
Expert consultation
Tension Pneumothorax
Needle decompression
Tube thoracostomy
Cardiac Tamponade
Pericardiocentesis
20 mL/kg NS/LR bolus
Pulmonary Embolism
20 mL/kg NS/LR bolus, repeat PRN
Consider thrombolytics, anticoagulants
Expert consultation
Hemodynamic Parameters in Shock
| Type | Examples | Preload (CVP, PCWP) |
Afterload (SVR) |
CO (SV*HR) |
Mixed Venous O2 (MVO2) | Management |
|---|---|---|---|---|---|---|
| Distributive | - Sepsis - Anaphylaxis - Severe neurologic injury (loss of α-1 activity) |
↓ | ↓ | ↑ then ↓ | ↑ | - Sepsis: Crystalloid (20 cc/kg NS, repeat PRN) + abx - Anaphylaxis: Epi + crystalloid - Neurogenic: Crystalloid + α-active pressors, (norepi @ 0.05-2 mcg/kg/min) |
| Hypovolemic | - Blood loss - GI or Renal losses - ↓ intake |
↑ | ↑ | ↑ | ↓ | - Crystalloid replacement: 20 cc/kg, repeat PRN - For blood loss: Consider pRBCs |
| Cardiogenic | - Myocarditis - MI - Dysrhythmia |
↑ | ↑ | ↑ | ↓ | Targeted at etiology: Inotropes, revascularization, anti-arrhythmics, cardiovert |
| Obstructive | - Tamponade - PE | ↑ | ↑ | ↑ | ↓ | Fix obstruction (pericardiocentesis, thrombectomy/lysis for PE) |
2.2.2 Respiratory Emergencies
Medications to Avoid in Children with Neuromuscular Disease
Recall that the use of succinylcholine for intubation of children w/ neuromuscular diseases may trigger life-threatening conditions, such as hyperkalemia or malignant hyperthermia. Several commonly used drugs, such as aminoglycosides, have intrinsic neuromuscular blocking activity that can worsen respiratory muscle weakness.
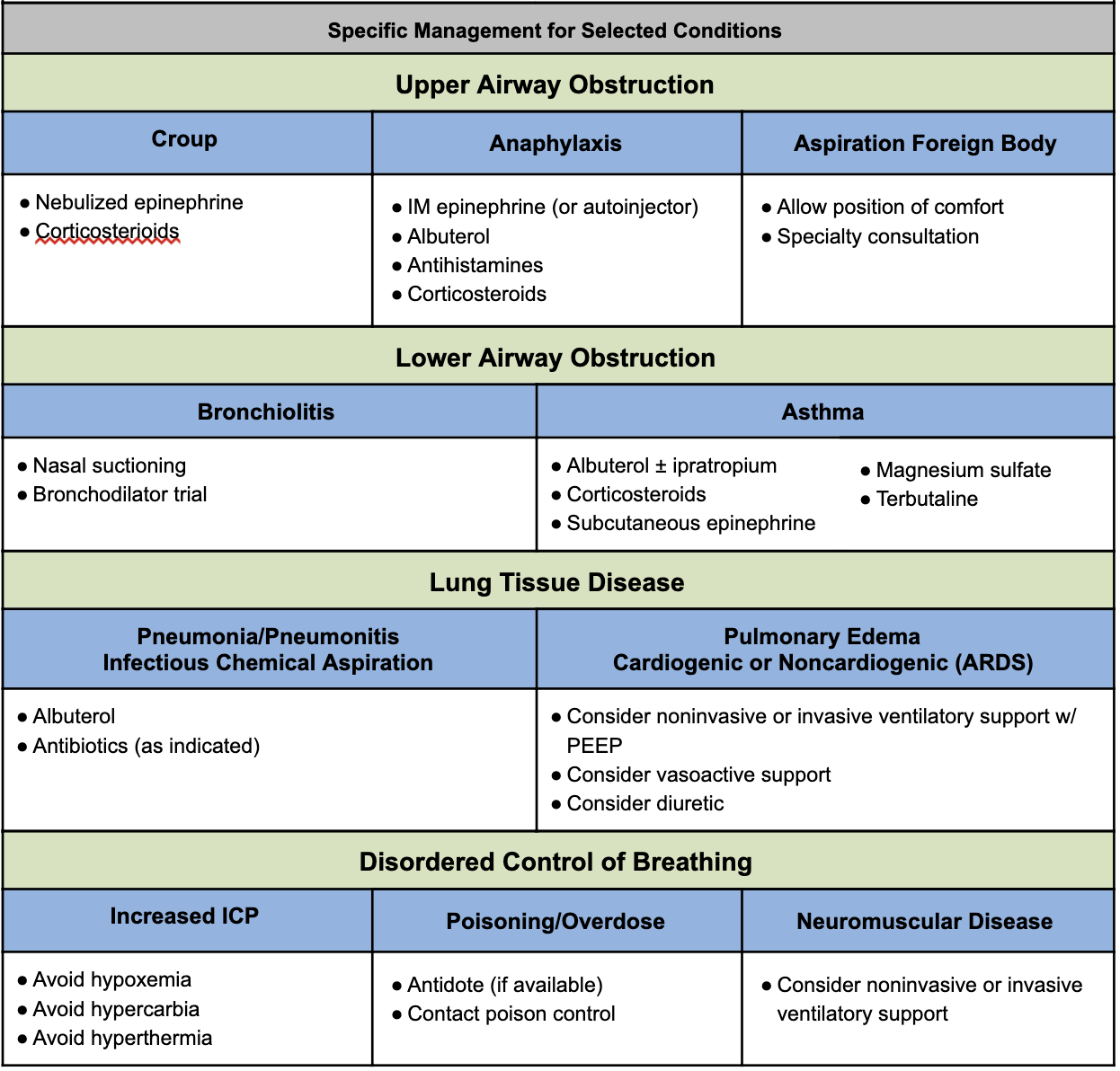
Management of Respiratory Emergencies Flowchart
Summarizes general management of respiratory emergencies and specific management by etiology. Note that this chart does not include all respiratory emergencies; it provides key management strategies for a limited number of diseases.
2.3 Infectious Disease
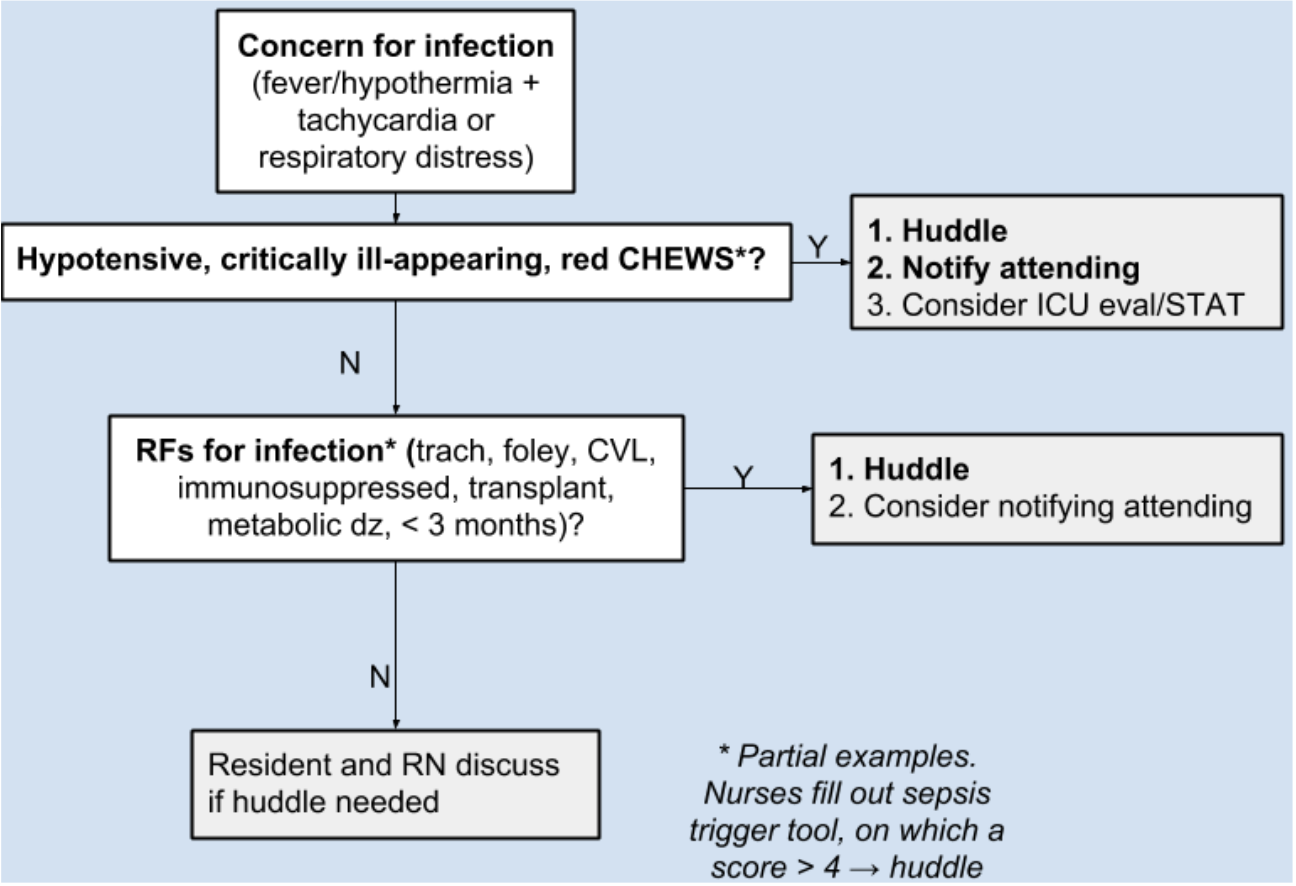
2.3.1 Sepsis Huddle
Huddle Steps
Resident Responsibilities
- Review vital sign trend
- Examine patient (especially respiratory, mental status, perfusion)
- Discuss IV access
- Review antibiotic plan: New agent(s) needed, delivery priority, need for ID consult
- Consider fluid bolus
- Discuss plan for repeat assessment
USE SEPSIS POWERPLAN TO ENSURE STAT IV ANTIBIOTICS AND FLUIDS!
2.3.2 CSF Analysis
Age-Based Ranges for CSF Studies
| Age | WBC (mm^3) Mean (Range) |
Glucose (mg/dL) Mean (Range) |
Protein (mg/dL) Mean (Range) |
|---|---|---|---|
| Premature | 9 | 50 (24-63) | 115 (65-150) |
| Term newborn | 8.2 (0-22) | 52 (34-119) | 90 (20-170) |
| 0-4 wks | 11 (0-35) | 46 (36-61) | 84 (35-189) |
| 4-8 wks | 7.1 (0-25) | 46 (29-62) | 59 (19-121) |
| >8 wks | 2.3 (0-5) | 61 (45-65) | 28 (20-45) |
2.3.2.1 General Heuristics for CSF Interpretation"
| Diagnosis | WBC | Glucose | Protein | Opening Pressure | Other |
|---|---|---|---|---|---|
| Bacterial meningitis | ↑, mostly PMNs | ↓ (<60% serum glucose) | ↑↑ | ↑ | +CSF Cx / gram stain, often +BCx |
| Viral meningitis | Slightly ↑, mostly lymphocytes | Normal | Normal to slightly ↑ | Normal | HSV may have RBCs in CSF |
| TB meningitis | ↑ (PMNs → lymphocytes) | ↓ (<60% serum glucose) | ↑ | Variable | +AFB |
| Fungal meningitis | ↑, lymphocytes | ↓ (<60% serum glucose) | ↑ | Variable | Fungal Cx |
| GBS | Normal | Normal | ↑↑ | Normal | So-called “albumino-cytologic dissociation” |
| SAH | Normal (accounting for peripheral ratio of RBC to WBC) | Normal | ↑ | Normal to ↑ | Xanthochromia = yellow appearance of CSF, suggests long-term presence of RBCs (to distinguish from traumatic tap) |
2.4 Respiratory
2.4.1 Status Asthmaticus
2.4.1.1 A-B-C
Epinephrine 0.01 mg/kg IM PRN extremis
2.4.1.2 Initial treatment
PowerPlans & Order Sets: ED Asthma Status Plan
“Unineb” = Albuterol + ipratropium combination nebs
- NOTE: 1x Unineb = 3x Combineb
Steroids (if no improvement after first neb or if patient on home steroids)
- Dexamethasone = dosed q24-48h, 0.6 mg/kg
- Prednisone/Prednisolone = dosed q12h, 2mg/kg
- Methylprednisolone 2mg/kg
2.4.1.3 If poor response, add
Magnesium sulfate 40mg/kg (2mg max)
- Monitor for hypotension, consider NS bolus
Continuous nebulized albuterol
- Titrate to HR
2.4.1.4 If poor response continues, add
Terbutaline: Loading dose 5-10 mCg/kg IV/SC over 10m. Infusion 0.4 mCg/kg/min IV.
- EKG, troponin, CK q12h
Consider Heliox 70:30 helium:oxygen mixture
2.4.1.5 If impending respiratory failure
- Rapid sequence intubation
- Mechanical ventilation: Minimize PEEP, maximize E time. Permissive hypercapnia. Anticipate air leak, pneumothorax, bronchospasm, PEA.
2.4.1.6 As patient improves
“Last on, first off” to peel off therapy
2.4.2 ABGs & VBGs
Presented as: pH / pCO2 / pO2 / HCO3
Venous pH + 0.035 = Arterial pH
Look at past VBGs for baseline pCO2 (e.g. chronically elevated in ex-preemies w/ CLD)
VBGs sufficient to assess acid-base status & clinical response to treatments (in general). ABG preferred over VBG:
- to accurately determine PaCO2 in severe shock
- to accurately determine PaCO2 if hypercapnic (i.e. PaCO2 >45 mmHg)
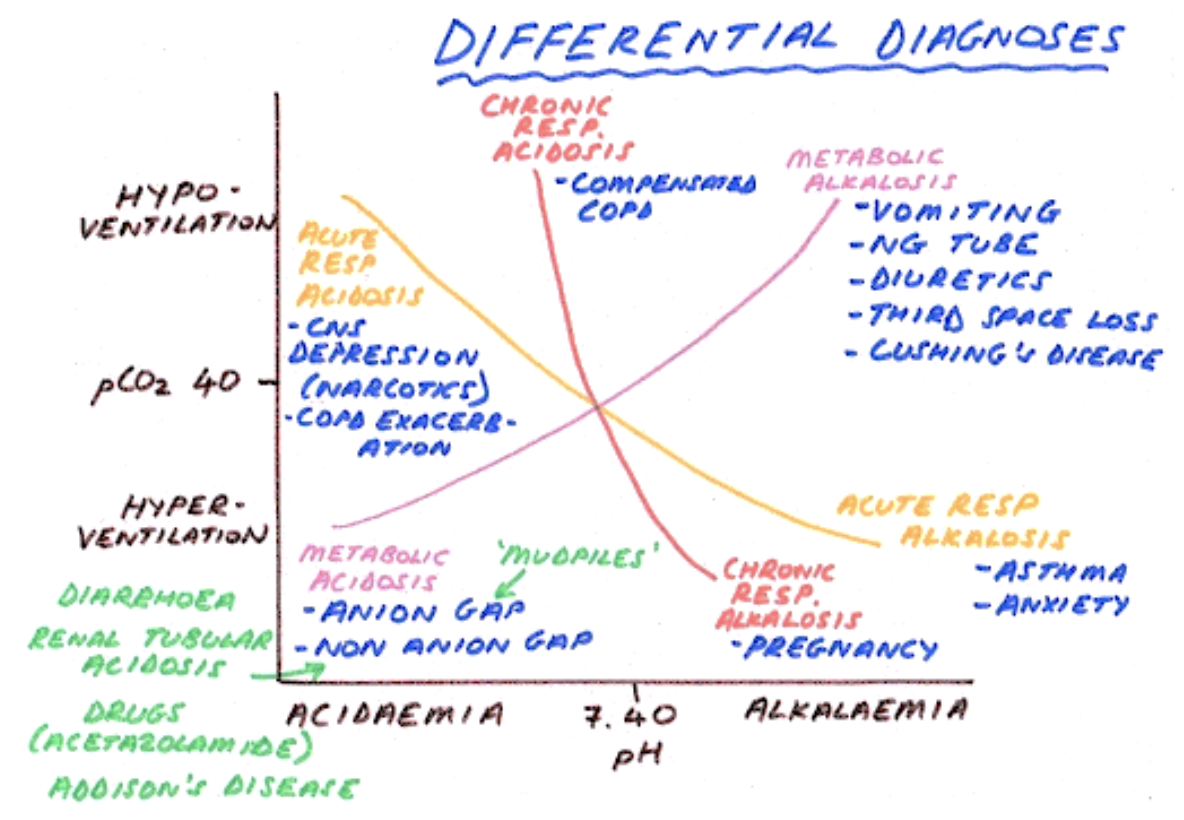
2.4.2.1 Stepwise Approach to ABG/VBG Interpretation
Compare pH to normal range
Identify the primary process that led to the change in pH (using PCO2/HCO3)
Calculate the serum anion gap (SAG)
- SAG = Na+ - (Cl- + HCO3-). If >12, there is a primary AG metabolic acidosis
Identify the compensatory process (if one is present)
Identify if any other disorders are present or there is a mixed acid-base process using delta/delta = (AG - 12) / (24 - Bicarb)
- < 0.4 → pure Non-AG Metabolic Acidosis (NAGMA)
- 0.4 - 0.8 → mixed NAGMA + High-AG Metabolic Acidosis (HAGMA)
- 0.8 - 2.0 → a pure HAGMA
- > 2.0 → mixed HAGMA + metabolic alkalosis
2.4.2.2 Normal Blood Gas Values
| Arterial | Venous | |
|---|---|---|
| pH | 7.35 - 7.45 | 7.31 - 7.41 |
| pCO2 (mmHg) | 35 - 45 | 40 - 50 |
| pO2 (mmHg) | 75 - 100 | 36 - 42 |
| HCO3 (meQ/L) | 22 - 26 | Same |
| BE | -2 to +2 | Same |
| O2 Saturation | >95% | 60-80% |
2.4.2.3 Compensation
| Disorder | Defect | Compensatory Response** |
|---|---|---|
| Respiratory Acidosis | ↑ pCO2 | ↑ HCO3 - Acute = +1 MeQ/L HCO3 for +10 mm Hg PaCO2 - Chronic = +4 MeQ/L HCO3- for +10 mm Hg PaCO2 |
| Respiratory Alkalosis | ↓ pCO2 | ↓ HCO3 - Acute = -2 MeQ/L HCO3 for -10 mm Hg PaCO2 - Chronic = -5 MeQ/L HCO3- for -10 mm Hg PaCO2 |
| Metabolic Acidosis | ↓ HCO3 | ↓ pCO2 - pCO2 = 1.5 x HCO3 + 8 +/- 2 (Winter’s Formula) |
| Metabolic Alkalosis | ↑ HCO3 | ↑ pCO2 - pCO2 + 0.6 for + 1.0 mEq/L HCO3 |
** HCO3 = kidneys (days). CO2 = lungs (minutes).
*** Limits of compensation: HCO3 = 15-38. CO2 = 10.
2.4.3 Respiratory Support for Spontaneously Breathing Patients
| Type | O2 Delivery | CO2 Exit | FiO2 | Rate | Pros | Cons |
|---|---|---|---|---|---|---|
| “Blow By” Oxygen (BBO2) | O2 tubing or simple mask held by a child’s face | Mouth | <30% (limited evidence) | At least 10L/min through a reservoir (such as mask) | Can be used in children who can’t tolerate other methods | Limited and variable O2 delivery |
| Low Flow Nasal Cannula (LFNC) | Through nasal prongs attached to tubing | Mouth | 25-40% (100% O2 delivers variable FiO2 based on placement of nares, patient’s inspiratory effort and minute ventilation) | 1-4L/min (Rates >2L/min can create Positive airway pressure in newborns/infants) | Mobile, infants can feed w/ low-flow in place, may be better tolerated than a mask | - Cannot reliably deliver high concentrations of FiO2 - Prongs can be difficult to keep in position |
| High Flow Nasal Cannula (HFNC) | Up to 8L/min in infants, up to 60L/min in children/adults | |||||
| Simple Mask | O2 enters mask through a tube | Holes in the side of the mask | 35-50% (Room air can enter through exit holes, mixing w/ delivered O2) | 6-10L/min | Can deliver higher concentrations of FiO2 than NC | Cannot reliably deliver precise concentrations of O2 because of mixing w/ room air |
| Partial Rebreather | O2 enters the mask through a tube as well as from an attached reservoir | Holes in the sides of the mask. Room air can still enter, but not as much as w/ the simple mask. | 50-60% O2 | 10-12L/min | ||
| Non-Rebreather Mask | O2 enters the mask through a tube as well as from an attached reservoir w/ a one-way valve | Two exhalation ports; one is fitted w/ a one-way valve and one allows mixing (fail-safe so that if the O2 delivery port blocked, patient doesn’t suffocate) | Up to 95% O2 | 10-15L/min | Max FiO2 administered to a spontaneously breathing patient | Stored in the code cart at BCH |
| CPAP/BiPAP | See Critical Care/ICP chapter |
| Type | O2 | CO2 Exit | FiO2 | Rate | Pros | Cons |
|---|---|---|---|---|---|---|
| “Blow By” Oxygen (BBO2) | O2 tubing or simple mask held by a child’s face | Mouth | <30% (limited evidence) | At least 10L/min through a reservoir (such as mask) | Can be used in children who can’t tolerate other methods | Limited and variable O2 delivery |
| Low Flow Nasal Cannula (LFNC) | Through nasal prongs attached to tubing | Mouth | 25-40% (100% O2 delivers variable FiO2 based on placement of nares, patient’s inspiratory effort and minute ventilation) | 1-4L/min (Rates > 2L/min can create Positive airway pressure in newborns/infants) Mobile, infants can feed w/ low-flow in place, may be better tolerated than a mask | Mobile, infants can feed w/ low-flow in place, may be better tolerated than a mask |
|
2.4.4 Trach Troubleshooting
2.4.4.1 Tracheostomy Basics
- Major types: Shiley or Bivona (more flexible, better for active children)
- Sizes: A “3.0” trach has an inner diameter of 3.0 mm, sizes vary by age
- Cuffed vs. uncuffed: Cuffs improve air seal and prevent aspiration, but uncuffed allows spontaneous breathing, improved vocalization, may be appropriate for infants and small children
- Outer vs. inner cannula: Outer cannula holds stoma open, inner cannula can be removed for cleaning
- Fenestration: Improves vocalization
- Trach ties: The part that wraps around the neck to keep trach in place
Trach Complications
Plan ahead!
- Differentiate new (< 7 days) vs. mature stoma (> 7 days)
- Know if your patient can be ventilated “from above” in event of trach malfunction
- Know your patient’s trach brand, size, features and have replacement trach at bedside, including one size smaller
Decannulation:
- Staff assist, call RT urgently
- If new stoma, do NOT blindly replace trach, call ORL instead
Obstruction:
- Mucous plugging → suction, replace inner cannula, etc.
- Back-walling = Distal end of trach obstructs against posterior tracheal wall → call RT, reposition trach, may need longer trach
- Tracheal stenosis or granulation tissue → call ORL, may need to be addressed surgically
- Consider deflating cuff and ventilating “from above” if possible
Bleeding:
- Although rare, have high index of suspicion for tracheo-arterial fistula, call ORL
- Differentiate blood from trach vs. from stoma/trach site
2.5 Status Epilepticus (SE)
2.5.1 PowerPlans & Order Sets
Neuro Seizure Admit Plan
2.5.2 Definition
- Neurologic emergency!
- Seizure lasting > 30 min or 2 sequential seizures w/o return to baseline
- Refractory SE is > 60 min
2.5.3 Presentation
Generalized SE, focal SE, hemi-convulsive status w/ hemiparesis
2.5.4 Differential
Sepsis, hypoglycemia, meningitis/encephalitis, skull fracture/trauma, HTN, mass, herniation
2.5.5 Management
Step 1 (0-5 min):
Monitors, O2, IV access, STAT labs (glucose, CBC, chem10, LFTs, UA/blood/urine cultures if febrile, urine tox screen, AED levels if relevant)
Lorazepam IV (0.1 mg/kg/dose. Max 4mg.)
If no access: Diazepam PR (0.5 mg/kg if <5yo; 0.3 mg/kg if 6-11yo; 0.2 mg/kg if >11yo)
- NOTE: Rapid redistribution → increased risk of seizure recurrence
Step 2 (10-15 min):
REPEAT Lorazepam IV (0.1 mg/kg/dose. Max 4mg.)
+ Fosphenytoin IV (20mg/kg infused over 7 min)
- NOTE: Will decrease BP
or Keppra IV (60 mg/kg IV. Max dose 4500 mg.)
Step 3 (20-30 min):
Consult Neurology. Consider LP, EKG.
Phenobarbital IV (20mg/kg infused over 15-20 min)
- NOTE: Will decrease RR, be prepared to intubate/bag
2.6 Psychiatric
2.6.1 Anxiety, Agitation & Delirium
2.6.1.1 Definition
Anxiety, agitation, and delirium can often present together and can be difficult to differentiate in the seriously ill child. Management is often similar.
2.6.1.2 Anxiety
Common among children with chronic or life-threatening illnesses. Difficult to separate from physical symptoms; may exacerbate physical symptoms (pain, dyspnea, etc).
2.6.1.3 Agitation
Unpleasant state of arousal → loud speech, crying, ↑ motor activity/autonomic arousal
2.6.1.4 Delirium
An acute-onset disturbance of consciousness that fluctuates throughout the day
2.6.1.5 Management
Non-pharmacologic: Treat underlying cause, meditation, diaphragmatic breathing, massage, biofeedback therapy, regulate sleep/wake cycle, frequent reorientation to time and place, frequent reassurance, minimize use of restraints
Pharmacologic
Ask Psych team when to use PO vs. IV/IM
Onset of action:
- PO/enteral: Usually 30-60 min for beginning of peak effects
- IM: Usually 15-30 min
- IV: Usually 5-15 min
| Drug | Dose | Notes |
|---|---|---|
| Diphenhydramine (Benadryl) | 1 mg/kg per dose PO/IM/IV - Limits per 24h: <=7yo: 50-75mg; 8-12yo: 75-100mg; Adolescents: 100-150mg |
- Anticholinergic - Avoid if dehydrated, CF, asthma, previous paradoxical rxn |
| Lorazepam (Ativan) | 0.02-0.05 mg/kg q6h PO/SL/IV/SC | |
| (8-12yo: ~0.5mg. 13yo+: 1mg.) - Limits per 24h: 8-12yo: 2mg; Adolescents: 3mg |
- Avoid in delirium - Avoid in pts <7yo |
|
| Clonidine | - <=7yo: 0.025-0.05mg first dose - 8-12yo: 0.05mg first dose 13yo+: 0.1mg first dose |
Useful w/ hx of ADHD, PTSD, younger children |
| Clonazepam | 0.005-0.01 mg/kg PO q8-12h - Can increase every 3 days up to 0.05-0.1 mg/kg PO q8-12h (max 0.2 mg/kg/day) |
Avoid in delirium |
| Haloperidol (Haldol) | 0.01-0.02 mg/kg PO q8h (max 0.5-1 mg) - Acute agitation: 0.025 mg/kg PO & can repeat 0.025 mg/kg in 1 hr as needed |
IM form for acute agitation, delirium, psychosis/mania |
| Risperidone | 0.25-0.5 mg PO qPM or divided (max 3 mg/day) | Order only w/ Psych input |
| Quetiapine (Seroquel) | 25 mg q12h PO, can increase daily by 25mg/dose, to max 100-200 mg q12h) | Order only w/ Psych input |
| Olanzapine (Zyprexa) | 1.2-2.5 mg PO daily (max 5 mg/day) | Order only w/ Psych input |
2.6.2 Overnight Behavioral Plan
- PowerPlans & Order Sets: Agitation (mild), agitation (moderate), agitation (severe), behavioral health safety plan, behavioral restraints
- Err on the side of more restrictive: When in doubt, put on a 1:1, order suicide precautions including finger foods, “arms length” if any significant concern for active attempts to hurt self, security at door for elopement risk, security in room if needs hands-on (care companion cannot put arms on/only observe and alert RN and team of concerns)
- Behavioral Rapid Response (BRR), Call 5-5555: For active unsafe behaviors. Summons BRT psych RN, on-call psychiatrist (if in-house), ER psych SW (if in-house).
- Never allow patient to get between you and the exit. Always ask for escort (including BRT clinician or PCS clinician). Put lanyards, long-hair, loose clothing away as able, etc.
- PGY-2s and above are the only people allowed to order physical or chemical IM restraints (must be 1-time orders, cannot write PRN IM psychotropic meds or PRN physical restraints)