26 Sports Medicine
26.1 General Approach to the MSK Exam
- History
- Mechanism, chronicity, exposures, associated symptoms
- Red flags: B symptoms, major trauma
- Inspection: Compare to contralateral side. Make sure to EXPOSE for best exam.
- Look for asymmetry, atrophy, deformity, ecchymosis, erythema, scars
- Red flags: Erythema (sign of infxn), deformity concerning for major trauma
- Palpation
- Feel for anatomic points of interest
- Red flags: Warmth (sign of infxn), diminished sensation (sign of neurologic deficit)
- Range of motion (ROM): Active first, then passive
- Look for pain w/ motion, limited ROM (and distinguish whether due to pain, effusion, mechanical problem)
- Strength
- Graded from 0-5 out of 5:
- 5/5 = full strength
- 4/5 = movement against some resistance
- 3/5 = movement against gravity
- 2/5 = movement but not against gravity
- 1/5 = muscle flicker
- 0/5 = no contraction
- Red flags: Diminished strength if not due to pain (sign of neurologic deficit)
- Graded from 0-5 out of 5:
- Special testing is joint specific - see relevant sections below
26.2 Fractures
26.2.1 Salter-Harris Classification for Physeal Fractures
| Type I | Type II | Type III | Type IV | Type V | |
|---|---|---|---|---|---|
| Lesion |  |
 |
 |
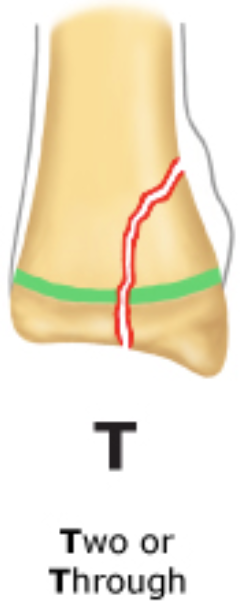 |
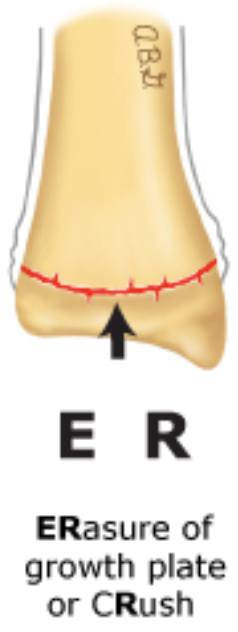 |
| Details | Often involves growth plate | Most common! Growth plate + metaphysis | Growth plate + epiphysis + joint space | Metaphysis + growth plate + epiphysis + joint space | Compression of growth plate |
| Implications | Good prognosis | Good prognosis | Threatens growth and articular integrity | Threatens growth and articular integrity | Very high risk for growth arrest |
| Management | - Dx: Usually clinical dx (XR negative unless displaced); contralateral XR may be useful - Immobilization (cast vs. splint) for > 3 wks |
Immobilization (cast vs. splint) for > 3 wks | - Immediate Ortho consult - Likely reduction (anatomic vs. surgical) |
- Immediate Ortho consult - Likely reduction (anatomic vs. surgical) |
- Immediate Ortho consult - Likely reduction (anatomic vs. surgical) |
26.3 Pre-Participation Physical
26.3.0.1 History
- Goal: Elucidate conditions that might preclude or limit sports participation
- Cardiac history
- Dyspnea on exertion → consider exercise induced asthma or vocal cord dysfunction
- History of head trauma
- History of “burners” or “stingers” (from transient brachial plexus compression/stretching) → if recurrent, may need C-spine XR
- Disordered eating (esp/ in sports w/ weight requirements)
- Substance abuse
- Family history: Sudden death, congenital heart disease, arrhythmias, Marfan syndrome
26.3.0.2 Physical Exam
Special attention to CV, resp, and MSK (assess ROM, symmetry, stability)
26.3.0.3 Cardiac Testing
- e.g. EKG, echo, exercise testing
- ONLY if clinically indicated, though highly controversial and recommendations worldwide differ. Current AHA/AAP PPE guidelines currently do not recommend global EKG/echo.
26.3.0.4 Clearance
- Increased risk of injury?
- Would treatment make athlete safe to participate?
- Can limited participation be allowed while treatment is undergone?
- Limitations for some or all sports?
26.4 Upper Extremity: Elbow, Forearm & Wrist
26.4.1 Anatomy
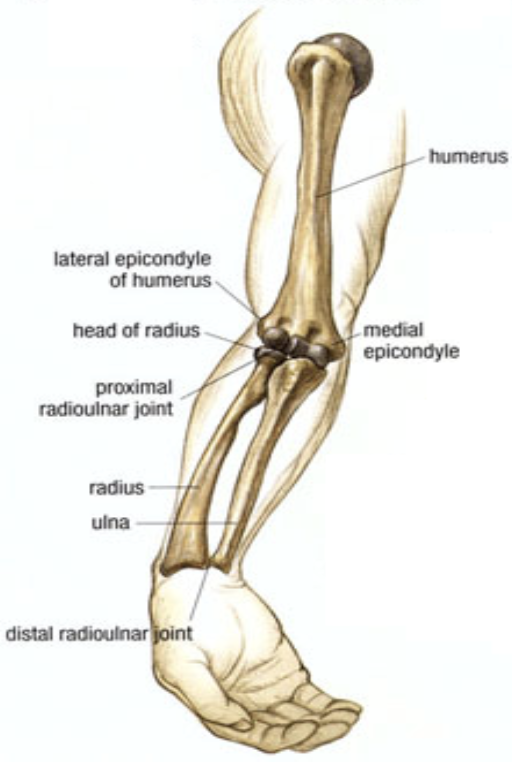
26.4.2 Exam Pearls
- Rapid elbow/forearm neurovascular exam:
- Brachial artery: Brachial + radial pulses, perfusion check
- Median nerve: Sensation over palmar side of digits 1-3
- Anterior interosseous nerve (motor-only branch of median nerve): “OK” sign 👌, grip strength
- Radial nerve: Wrist extension, thumbs-up sign 👍
- Ulnar nerve: Spread fingers against resistance
26.4.3 Supracondylar Fracture
26.4.3.1 Description/Mechanism
Usually fall on outstretched hand (FOOSH) with elbow hyperextension
26.4.3.2 Diagnosis
- Exam: Gross deformity, limited active elbow motion
- Imaging: AP + lateral XR. Findings may be subtle (posterior fat pad sign on lateral film)
26.4.3.3 Management
- Ortho consult
- Usually surgical fixation for displaced fractures
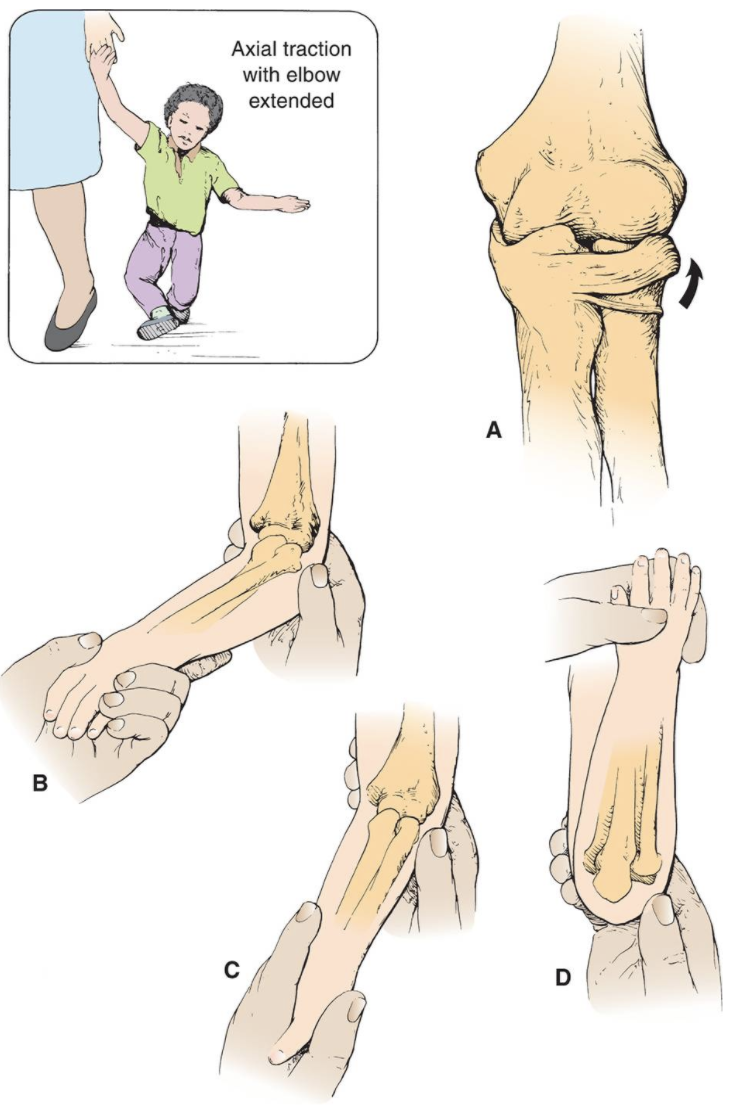
26.4.4 Nursemaid’s Elbow (Subluxation of Radial Head)
26.4.4.1 Description/Mechanism
Traction on arm with extended elbow (e.g. swinging child through the air)
26.4.4.2 Diagnosis
- Exam: No deformity, elbow held in passive pronation with slight flexion, refusing to use arm
- Imaging: Unnecessary unless suspect fracture based on H&P, or if reduction unsuccessful
26.4.4.3 Management
Stabilize elbow w/ one hand → supinate forearm and flex elbow (will usually feel/hear click)
26.4.5 Distal Radius Fracture
26.4.5.1 Description/Mechanism
- FOOSH
- Most common pediatric fracture
26.4.5.2 Diagnosis
- Exam: Pain, ecchymosis, swelling
- Imaging: AP + lateral XR of wrist and forearm; consider AP + lateral of elbow if tender or if diaphyseal fractures present
26.4.5.3 Management
- Ortho consult
- Depending on severity, may require anything from immobilization to ORIF
26.5 Upper Extremity: Shoulder
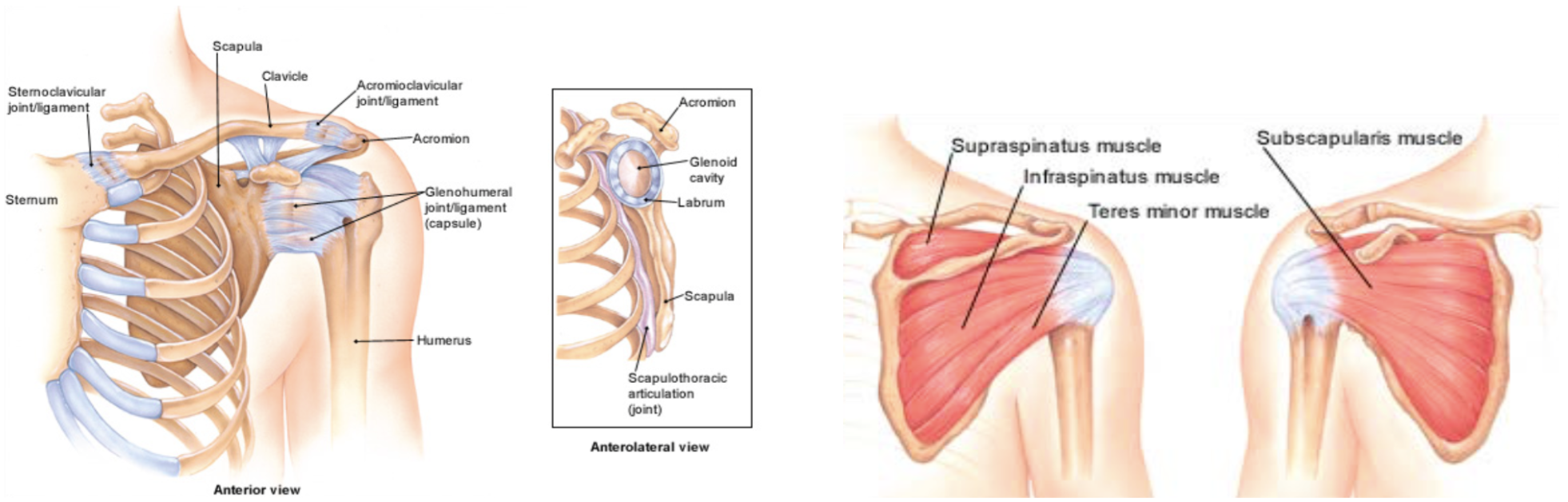
26.5.1 Anatomy
- Rotator cuff muscles (mnemonic: SITS → AEEI)
- Supraspinatus → Abduction
- Infraspinatus and Teres Minor → External rotation x2
- Subscapularis → Internal rotation
26.5.2 Exam Pearls & Special Tests
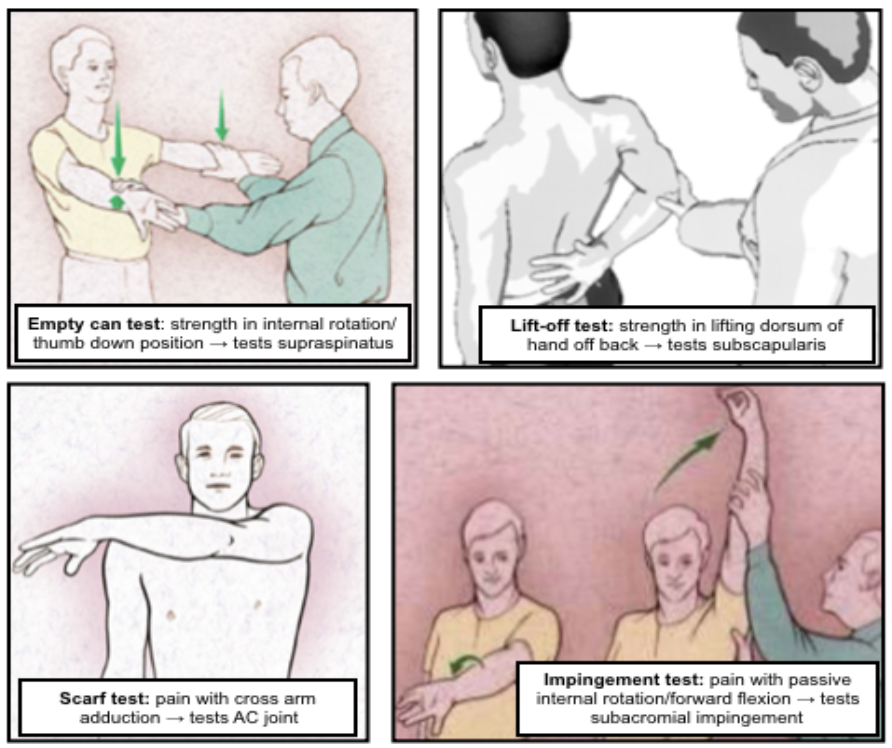
- Empty can test: Strength in internal rotation/thumb down position. Tests supraspinatus.
- Scarf test: Pain w/ cross arm adduction. Tests AC joint.
- Lift-off test: Strength in lifting dorsum of hand off back. Tests subscapularis.
- Impingement test: Pain w/ passive internal rotation/forward flexion. Tests subacromial impingement.
26.5.2.1 Common Associations
- Scapular winging i/s/o recent trauma or viral illness → likely serratus anterior or trapezius dysfunction
- Inability to passively/actively rotate affected arm externally s/p seizure → likely posterior shoulder dislocation
- Supraspinatus/infraspinatus wasting → likely rotator cuff tear or suprascapular nerve entrapment
- Decreased cervical ROM w/ pain radiating below elbow → likely cervical disc disease
- Shoulder pain in a throwing athlete w/ anterior glenohumeral joint pain/impingement → likely glenohumeral joint instability
- Pain or “clunking” sound w/ overhead motion → likely labral disorder
26.5.3 Proximal Humeral Fracture
26.5.3.1 Description/Mechanism
- FOOSH
- Direct blow to lateral shoulder
26.5.3.2 Signs & Symptoms
History of trauma, severe shoulder pain, pain w/ arm movement
26.5.3.3 Diagnosis
- Exam: tenderness, swelling, shoulder asymmetry, arm shortened and held in extension
- Imaging: AP + axillary XR of humerus
- Also get scapular “Y” view if concerned for shoulder injury
- Suspect Salter-Harris I if negative XR + tenderness at physis
26.5.3.4 Management
- Immobilization
- Likely Ortho consult, esp. if more severe (a/w shoulder dislocation, neurovascular compromise, etc.)
26.5.4 Dislocation
26.5.4.1 Description/Mechanism
- Majority of dislocations are anterior
- Blow to abducted/externally rotated/extended arm
- FOOSH
- Forceful forward swinging of arm
26.5.4.2 Diagnosis
- Exam: Arm abducted and externally rotated w/ resistance to all movement, loss of rounded appearance of shoulder. Evaluate for sensory loss over lateral deltoid (2/2 axillary nerve dysfunction).
- Imaging: AP + scapular “Y” + axillary XR to confirm dx and exclude fractures (can be repeated post-reduction if unsure of success)
26.5.4.3 Management
Reduction (variety of techniques exist) → immobilization and referral to Sports Med/Ortho for prevention of recurrent dislocation
26.5.5 Rotator Cuff Injury
26.5.5.1 Description/Mechanism
- Includes impingement (inflammation & pinching of rotator cuff tendons) and rotator cuff tears
- Impingement very common, tears very uncommon in youth athletes
- Overuse or acute injury, usually involving throwing or overhead activities
26.5.5.2 Signs & Symptoms
Pain in upper arm, worse w/ overhead activity or lying on affected side
26.5.5.3 Diagnosis
- Exam: Pain/weakness w/ testing of rotator cuff muscles; positive empty can, lift off, Hawkins, and/or impingement tests (see above)
- Imaging: XR only if bony pathology suspected; MRI best
26.5.5.4 Management
- Can start w/ conservative management (NSAIDs, PT)
- Chronic, symptomatic tears → consider surgical intervention
26.5.6 Little Leage Shoulder (Proximal Humeral Epiphysiolysis)
26.5.6.1 Description/Mechanism
- Overuse injury from throwing causing microfractures in humeral epiphysis
- Most common in 11-16yo athletes
26.5.6.2 Signs & Symptoms
Progressive shoulder pain w/ throwing, localized to proximal humerus, usually lateral
26.5.6.3 Diagnosis
- Exam: TTP at proximal lateral humerus over deltoid
- Imaging: AP XR of both arms in external and internal rotation; can get MRI if dx unclear
26.5.6.4 Management
- Rest x3 mos (minimum) + PT, then gradual progression to throwing
- Can still bat and play positions that do not require a lot of throwing
26.5.7 Acromioclavicular (AC) Joint Injury
26.5.7.1 Description/Mechanism
- Ranges from sprain of AC ligaments to full ligamentous rupture w/ clavicular displacement
- Usually fall onto or direct blow to shoulder
26.5.7.2 Diagnosis
- Exam: Tenderness, swelling, asymmetry at AC joint, prominent distal clavicle; + scarf test
- Imaging: XR (abnormal in more severe injury, may be normal if joint space not widened)
26.5.7.3 Management
- Less severe injury (no separation of joint capsule) → sling 1-2 wks, ice, NSAIDs → early motion as able, including flexion/extension at elbow
- More severe injury → likely surgical intervention
26.5.8 Clavicular Fracture
26.5.8.1 Description/Mechanism
Classified by location: most common is midshaft fracture > distal third > proximal third
26.5.8.2 Diagnosis
- Exam: Arm held adducted close to body, often supported w/ opposite hand; point tenderness, crepitus
- Neurovascular and respiratory exam crucial due to risk of brachial plexus and lung injury
- Imaging: XR
26.5.8.3 Management
- Most heal well w/ sling, but indications for surgery are controversial
- Any sign of neurovascular compromise → acute reduction needed
26.6 Lower Extremity: Hip
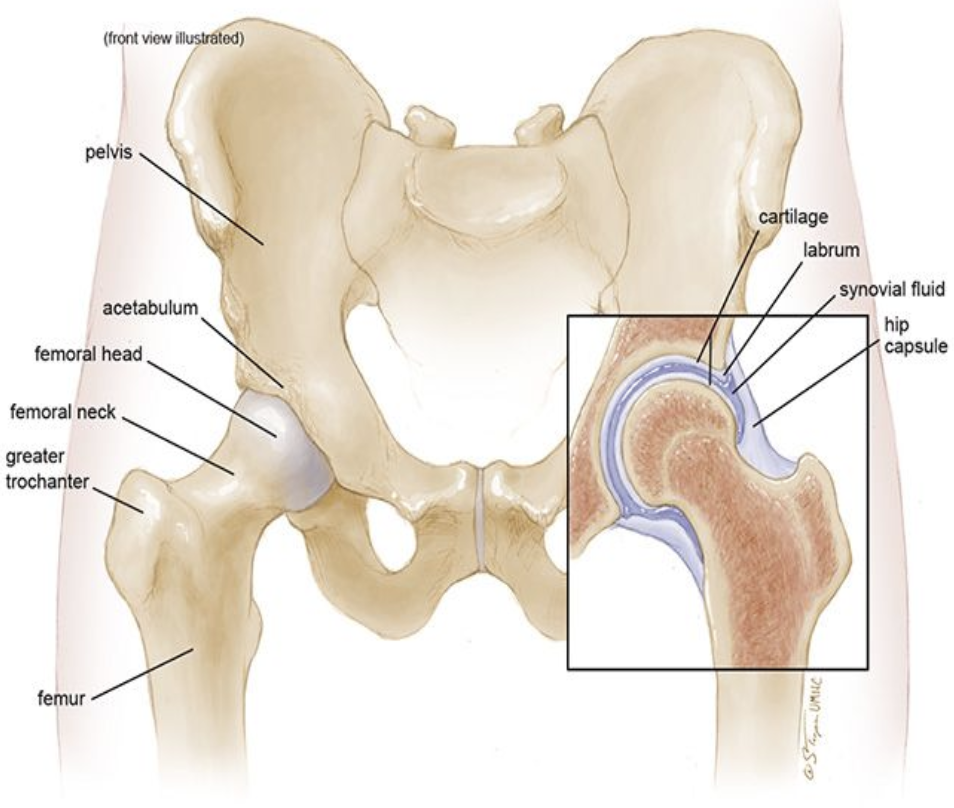
26.6.1 Anatomy
26.6.2 Exam Pearls & Special Tests
- Hip pain can refer to groin, thigh, or knee, or can present as limp/refusal to walk w/o complaint of pain
- Pain from intra-articular pathology often localizes to groin
- Barlow/Ortolani: Remember to apply gentle anterior pressure to the trochanter during abduction (Ortolani test)
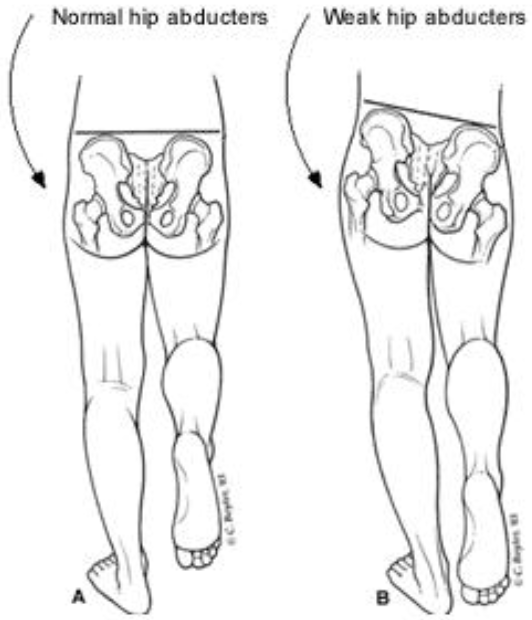
- Trendelenburg test: Positive when patient stands on one leg and the contralateral hip drops, indicative of gluteals/hip abductor weakness
- FABER (Flexion, Abduction, External Rotation): Test for hip or SI joint pathology
- FADIR (Flexion, Adduction, Internal Rotation): Test for hip impingement
- Log roll test: Patient on back w/ leg fully extended and relaxed, examiner passively rotates leg and hip internally and externally. Pain should yield high suspicion for intra-articular pathology.
26.6.3 Legg-Calve-Parthes Disease
26.6.3.1 Description/Mechanism
- Avascular necrosis (AVN) of the hip
- Most common age 5-7yo, M > F, bilateral in 10-20%
26.6.3.2 Signs & Symptoms
Activity-related hip pain and/or limp (acute or chronic)
26.6.3.3 Diagnosis
- Exam: Trendelenburg gait, decreased hip abduction and internal rotation
- Imaging: XR often normal early in course, bone scan or MRI more suggestive of dx
26.6.3.4 Management
- Non-weight bearing and restoration of motion (crutches), NSAIDS, PT, aquatherapy
- Severe cases may require spica casting or surgery
26.6.4 Slipped Capital Femoral Epiphysis (SCFE)
26.6.4.1 Description/Mechanism
- Displacement of the capital femoral epiphysis from the femoral neck through the physeal plate
- Commonly ages 10-16yo, M > F, bilateral in 20-40%
26.6.4.2 Signs & Symptoms
Groin pain, knee pain, limp
26.6.4.3 Diagnosis
- Exam: Decreased hip ROM, hip externally rotated at rest, leg length discrepancy
- Imaging: AP + frog leg lateral hip XR. Look for “ice cream scoop falling off the cone, S-sign (frog leg) + Klein’s Line (AP) for subtle cases.

26.6.5 Developmental Dysplasia of the Hip (DDH)
26.6.5.1 Description/Mechanism
- Abnormal development of shallow acetabulum causing hip joint instability
- F > M
26.6.5.2 Diagnosis
- Exam: Positive Barlow/Ortolani (only reliable in ages <3mo). Limitation of hip abduction or positive Galeazzi (asymmetric knee heights when hips & knees flexed) in ages >3mo.
- Imaging: US until age 4-6mos, AP XR pelvis w/ hip in 20-30 degree flexion after age 4-6mos
26.6.5.3 Management
- Ortho referral
- Depending on age at diagnosis/referral and severity, may be treated w/ anything from observation to harness to operative management
26.6.6 Femoroacetabular Impingement (FAI)
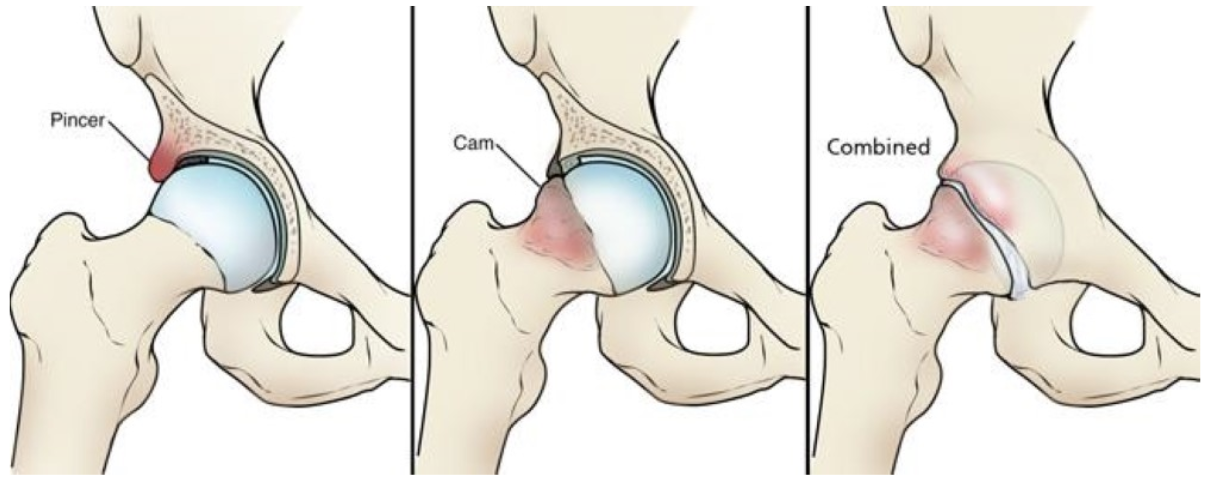
26.6.6.1 Description/Mechanism
- Trapping of femoral neck against anterior acetabulum
- Acetabular overcoverage (Pincer impingement) vs decreased head-neck offset (CAM impingement) vs both
- Common in athletes
- Difficult to differentiate from hip flexor tendinitis
26.6.6.2 Diagnosis
- Exam: Pain on hip flexion passively or against resistance, impact/running, deep flexion; pain is usually anterior or into groin.
- Imaging: XR AP Pelvis and Dunn laterals bilaterally
- Can have skeletal setup and still not be their pain cause
26.6.6.3 Management
Safe to start with PT unless having mechanical/catch/lock symptoms or difficulty weight bearing (in which case, refer to Sports Med/Ortho)
26.7 Lower Extremity: Knee
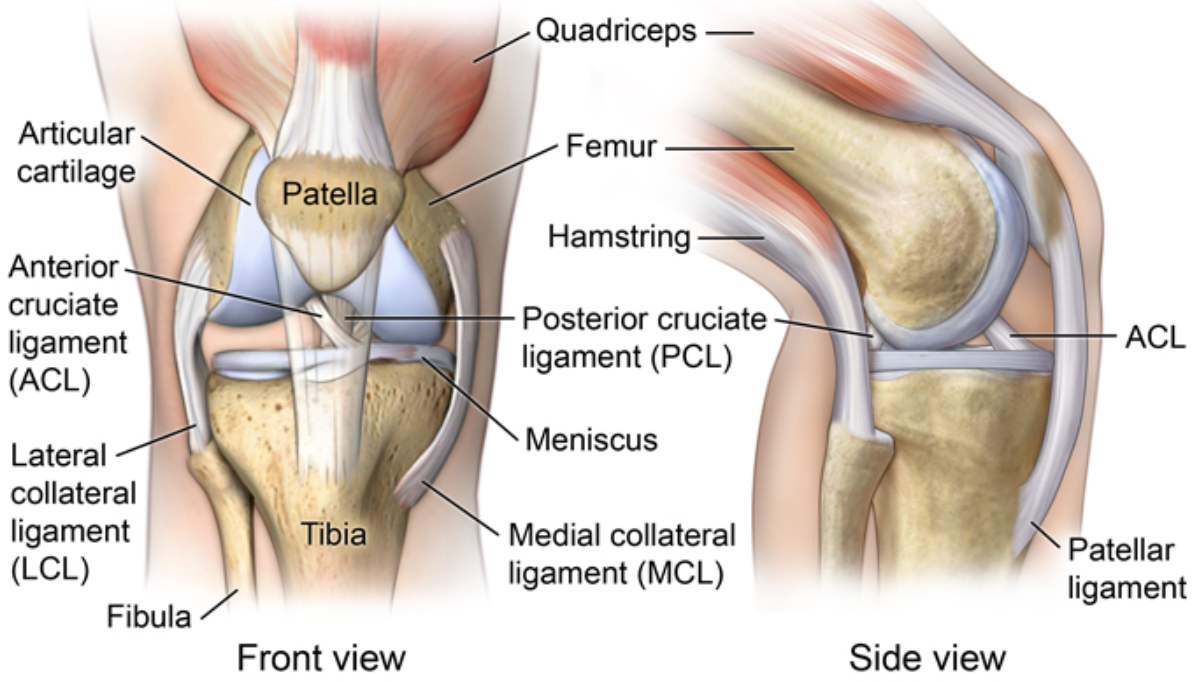
26.7.1 Anatomy
26.7.2 Exam Pearls & Special Tests
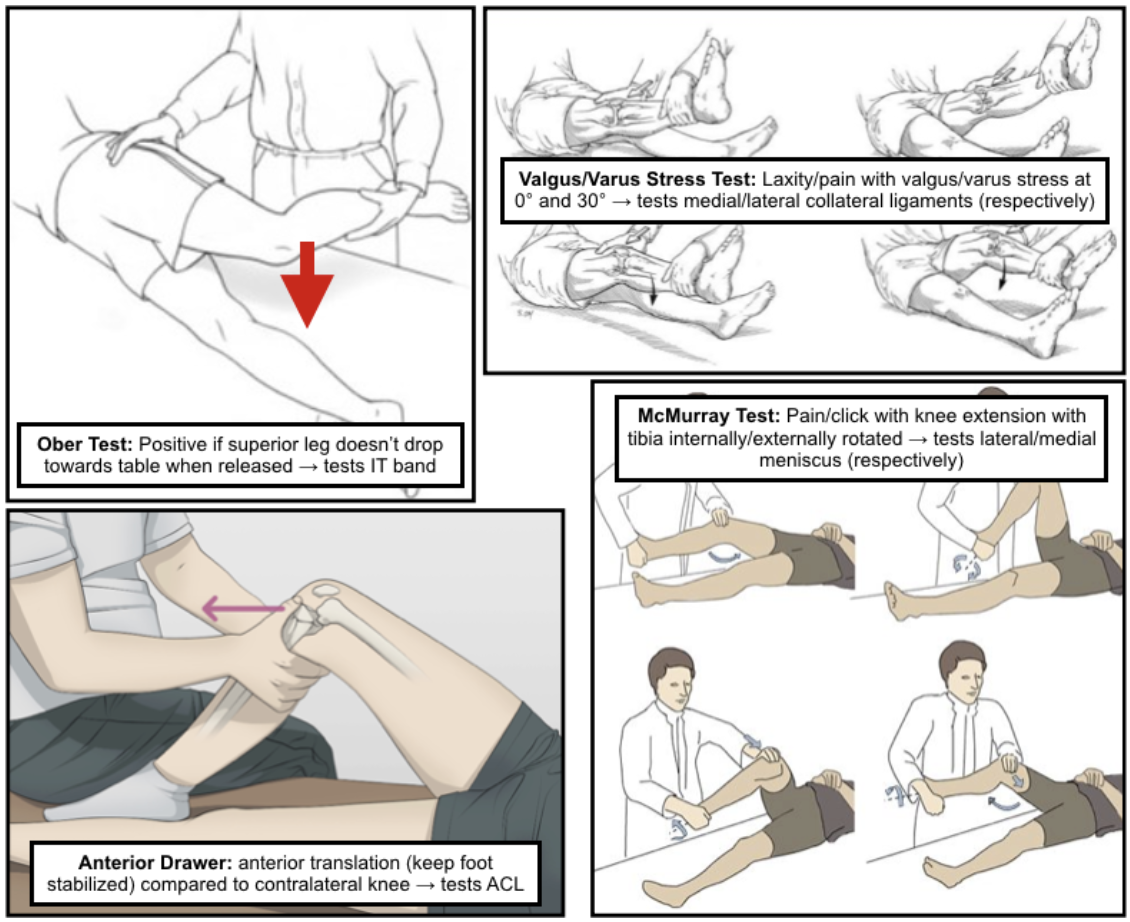
- Ober test: Positive if superior leg doesn’t drop towards table when released. Tests IT band.
- Anterior drawer test: Anterior translation (keep foot stabilized) compared to contralateral knee. Tests ACL.
- Valgus/varus stress test: Laxity/pain w/ valgus/varus at 0° and 30°. Tests MCL/LCL (respectively).
- McMurray test: Pain/click w/ knee extension w/ tibia internally/externally rotated. Tests lateral/medial meniscus (respectively).
26.7.3 Osgood-Schlatter Disease
26.7.3.1 Description/Mechanism
- Traction apophysitis of tibial tubercle at patellar tendon insertion
- Often children who play jumping sports and/or are undergoing rapid growth spurt
- Corollary process at inferior patellar pole = Sinding-Larsen-Johansson Syndrome
26.7.3.2 Signs & Symptoms
- Gradually worsening anterior knee pain, exacerbated by kneeling, jumping, stairs, walking uphill
- Can be asymmetric or bilateral
- Pain relieved by rest
26.7.3.3 Diagnosis
- Exam: Prominence of and TTP at the tibial tubercle, pain w/ resisted knee extension or squatting
- Imaging: Not routinely indicated unless to rule out other dx
26.7.3.4 Management
- Usually conservative: Pain management, PT for strengthening
- Continuation of activity, as long as not prolonged squatting/kneeling (e.g. playing)
26.7.4 Patellofemoral Pain Syndrome (PFPS)
26.7.4.1 Description/Mechanism
Abnormal tracking of patella causes anterior knee pain w/o intra-articular pathology
26.7.4.2 Signs & Symptoms
- Anterior knee pain worsened w/ prolonged sitting (theater sign) or descending stairs
- Pain w/ running/impact activity (aka Runner’s knee)
26.7.4.3 Diagnosis
- Exam: Positive J-sign (lateral patellar tracking during terminal knee extension), positive patella mobility test (medial glide < ¼ or > ¾ patella width suggesting hypo- or hypermobility)
- Imaging: Not routinely indicated unless to exclude other dx
26.7.4.4 Management
- Conservative treatment, PT for strengthening
- Avoid long-term NSAID use
26.7.5 Anterior Cruciate Ligament (ACL) Injuries
26.7.5.1 Description/Mechanism
- Cutting/pivoting motion causing valgus stress on knee, can be due to direct blow causing hyperextension/valgus deformation
- Medial meniscus and MCL often injured at same time (Unhappy Triad)
26.7.5.2 Signs & Symptoms
“Pop” at time of injury, swelling, feeling of knee “giving out”
26.7.5.3 Diagnosis
- Exam: Joint effusion, positive anterior drawer test
- Imaging: MRI > XR, but can get XR to evaluate for associated injury/fracture
26.7.5.4 Management
- Ortho/Sports Med referral
- Operative management in majority of cases, ideally w/ period of pre-operative rehabilitation to optimize outcomes
26.7.6 Meniscus Injuries
26.7.6.1 Description/Mechanism
- Direction change w/ knee rotation, planted foot, and flexed knee
- Commonly in sports w/ lots of deceleration and direction change
26.7.6.2 Signs & Symptoms
- Often insidious onset of pain/swelling in 24h after injury
- Pain worse w/ twisting/pivoting
- Can have locking/popping/catching sensation
26.7.6.3 Diagnosis
- Exam: Joint line tenderness, inability to fully extend/squat/kneel, positive McMurray test
- Imaging: MRI > XR (plain films often negative)
26.7.6.4 Management
- Ortho/Sports Med referral
- Management varies from conservative to operative (usually arthroscopic)
26.7.7 Iliotibial (IT) Band Syndrome
26.7.7.1 Description/Mechanism
Tight IT band sliding over lateral femoral epicondyle
26.7.7.2 Signs & Symptoms
Diffuse lateral knee pain, worsened w/ activity or w/ prolonged sitting w/ knee in flexed position
26.7.7.3 Diagnosis
- Exam: TTP in lateral knee, positive Ober test
- Imaging: Not routinely indicated
26.7.7.4 Management
- Activity modification
- NSAIDs
- Stretching/strengthening regimen
26.7.8 Osteochondritis Dissecans
26.7.8.1 Description/Mechanism
- Acquired subchondral bone lesion which can progress to involve cartilage causing separation from underlying bone; most common in knee
- Mechanism unknown; proposed to be due to repetitive trauma vs. inflammation
- Can lead to osteoarthritis if not recognized/treated
26.7.8.2 Signs & Symptoms
- May be incidental finding on imaging vs. non-specific activity related knee pain
- May have swelling or symptoms of catching/locking if lesions are unstable
26.7.8.3 Diagnosis
- Exam: No specific findings
- Imaging: 4-view XR (AP, lateral, sunrise, tunnel) of knee, MRI to further delineate known OCD lesion and determine management (or if XR negative but high clinical suspicion)
26.7.8.4 Management
- Referral to Ortho/Sports Med
- May be treated conservatively (non-weight-bearing or activity limitation) vs. operatively (if lesions are unstable or unresponsive to conservative treatment)
26.8 Lower Extremity: Ankle/Foot
26.8.1 Anatomy
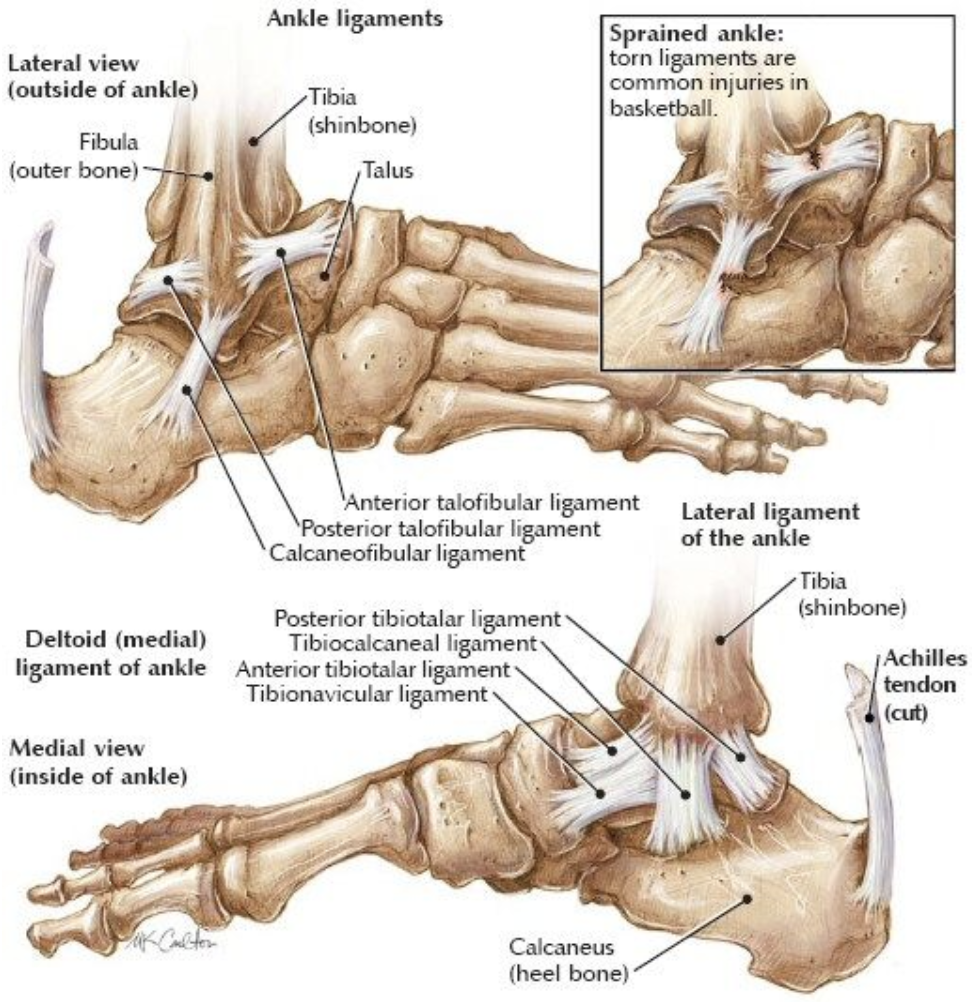
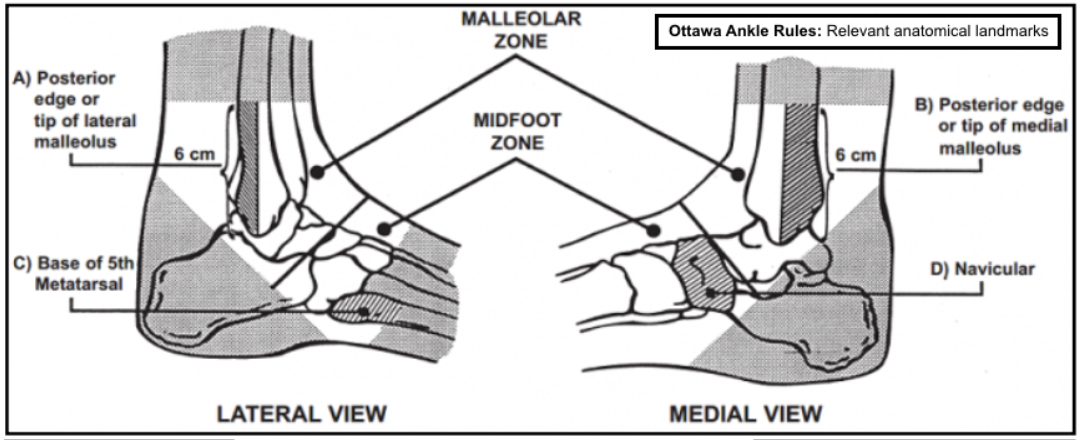
26.8.2 Exam Pearls & Special Tests
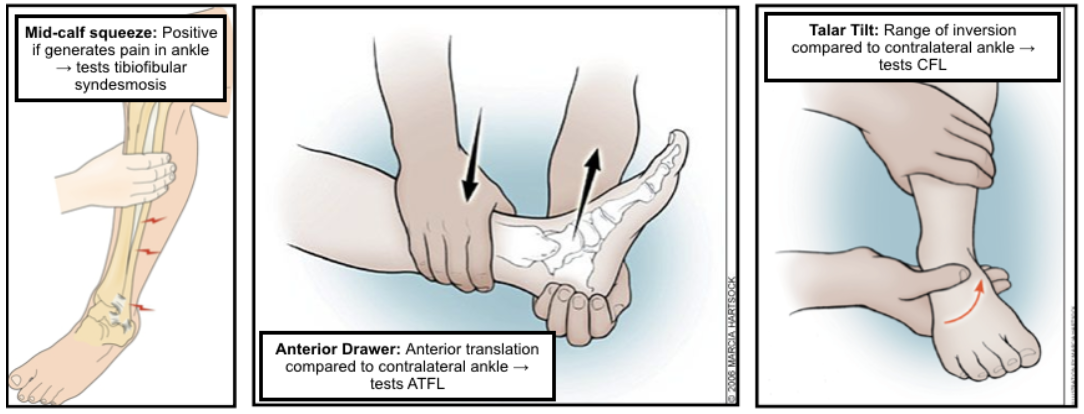
- Mid-calf squeeze: Positive if generates pain in ankle. Tests tibiofibular syndesmosis.
- Anterior drawer test: Anterior translation comapred to contralateral ankle. Tests ATFL.
- Talar tilt: Range of inversion compared to contralateral ankle. Tests CFL.
- Ottawa ankle rules (when to get XR of ankle/foot, validated for >18yo):
- Ankle: Pain in malleolar zone + EITHER of:
- Bony tenderness at posterior edge of lateral/medial malleolus
- Inability to bear weight both immediately after injury + at time of exam
- Foot: Pain in midfoot zone + EITHER of:
- Bony tenderness at base of 5th metatarsal or navicular bone
- Inability to bear weight both immediately after injury + at time of exam
- Ankle: Pain in malleolar zone + EITHER of:
26.8.3 Ankle Sprain
26.8.3.1 Description/Mechanism
- Ligamentous stretching/tearing
- Lateral: Inversion of plantar-flexed foot; injuries ATFL most commonly
- Medial: Eversion or abduction/ external
26.8.3.2 Signs & Symptoms
Pain, swelling (diffuse or localized), +/- inability to bear weight
26.8.3.3 Diagnosis
- Exam: Swelling, TTP, positive anterior drawer/talar tilt (lateral sprain), positive mid-calf squeeze (high sprain), squeeze test for syndesmotic injury
- Imaging: Not routinely indicated unless concern for fracture (see Ottawa rules above) or clinical uncertainty
26.8.3.4 Management
- Short period of complete immobilization (longer depending on severity), supportive device (lace-up brace or elastic bandage)
- ROM/strength exercises (can be w/ formal PT, esp. in case of recurrent ankle sprains) are critical to restoring function and proprioception
- For HIGH ankle sprains, consult Ortho/Sports Med (may need acute surgical stabilization if severe)
26.8.4 Sever’s Disease
26.8.4.1 Description/Mechanism
- Traction apophysitis of calcaneal growth plate at site of Achilles insertion; often children who play sports w/ jumping/heel striking and/or are undergoing rapid growth spurt
- Essentially Osgood-Schlatter at the calcaneus
26.8.4.2 Signs & Symptoms
Chronic heel pain w/ insidious onset, worse w/ activity or wearing non-supportive footwear
26.8.4.3 Diagnosis
- Exam: TTP at calcaneal apophysis or w/ “calcaneal compression test”
- Imaging: Not routinely indicated unless diagnosis unclear or to rule out fracture
26.8.4.4 Management
Painful activity → gradual return to play, use of heel cup for support, ice and stretching
26.8.5 Spiral/Oblique Fracture
26.8.5.1 Description/Mechanism
- “Toddler’s fracture” in 9mo-3yo
- Rotation around fixed foot → distal tibial fracture; often minimal trauma in toddlers, higher impact injury in older children
- ~30% of tibial fractures have associated fibular fracture
- Spiral fractures in NON-ambulatory child → concern for NAT
26.8.5.2 Signs & Symptoms
Limp, refusal to bear weight
26.8.5.3 Diagnosis
- Exam: Point tenderness over distal ⅓ of tibia
- Imaging: AP + lateral XR of the tibia and fibula; fractures may be occult (not seen on imaging)
26.8.5.4 Management
- Immobilization in long leg posterior splint/cast
- Ortho referral
26.8.6 Congenital Clubfoot
26.8.6.1 Description/Mechanism
- Idiopathic vs. due to intrinsic (e.g. neurologic) or extrinsic (e.g. fibroids) factors
- 1:1000 live births, M > F
26.8.6.2 Diagnosis
- Exam: Fixed (e.g. not correctable) deformity of the foot w/ plantar flexion and inversion + rotation, calf atrophy
- Imaging: Usually dx on prenatal US, XR minimally useful initially
26.8.6.3 Management
- Ortho referral (usually done in nursery prior to d/c)
- Serial casting → Achilles tenotomy → bracing
26.9 Spine
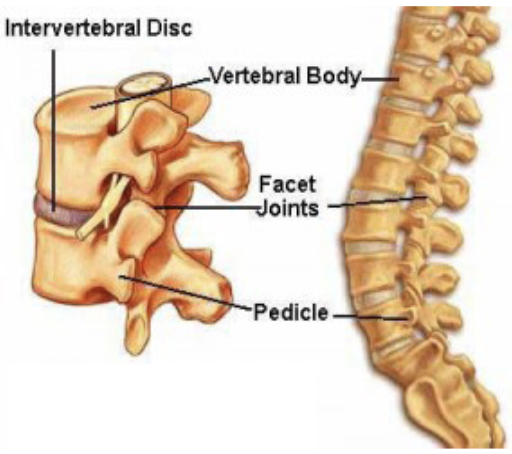
26.9.1 Anatomy
26.9.2 Exam Pearls & Special Tests
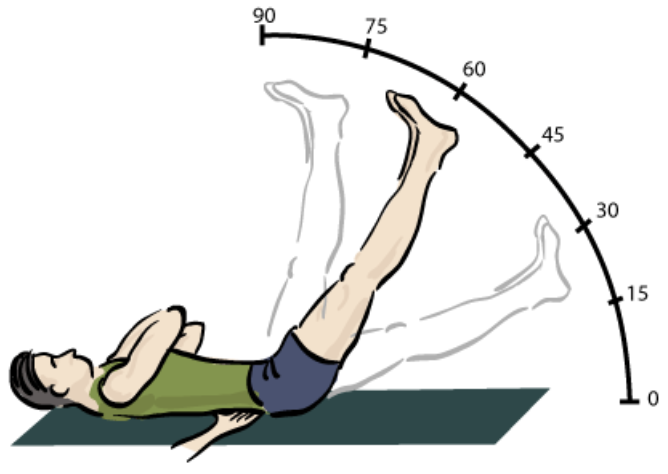
- Straight leg raise: Patient lying supine → flex at hip w/ knee straight (best if cervical spine flexed and ankle dorsiflexed) → assess for sciatic pain (sign of herniated disc)
26.9.3 Scoliosis
26.9.3.1 Description/Mechanism
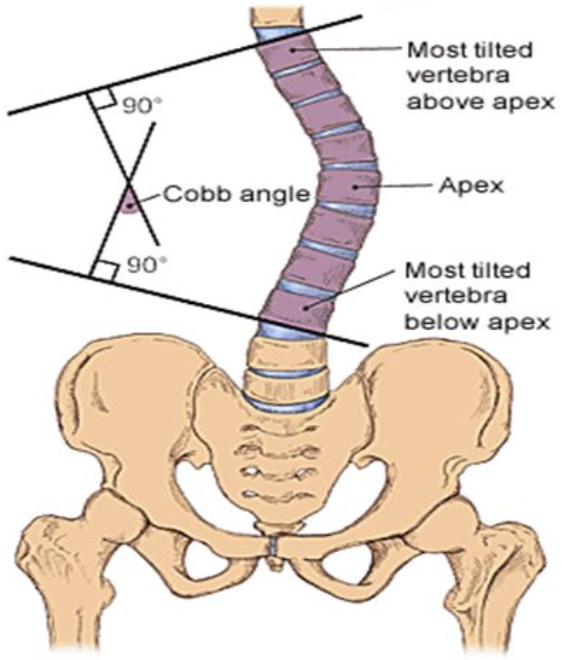
- Lateral curvature of the spine > 10°
- Idiopathic (80%) vs. congenital vs. neuromuscular
26.9.3.2 Diagnosis
- Exam: Adam’s forward bend test + inclinometer. Shoulder/torso asymmetry, rib prominence, paraspinal muscle prominence.
- Imaging: XR w/ Cobb Angle > 10°
26.9.3.3 Management
- Less than 25° → observation
- 25-45° + skeletal immaturity → bracing
- Greater than 45° → consider surgical intervention
26.9.4 Spondylolysis & Spondylolisthesis
26.9.4.1 Description/Mechanism
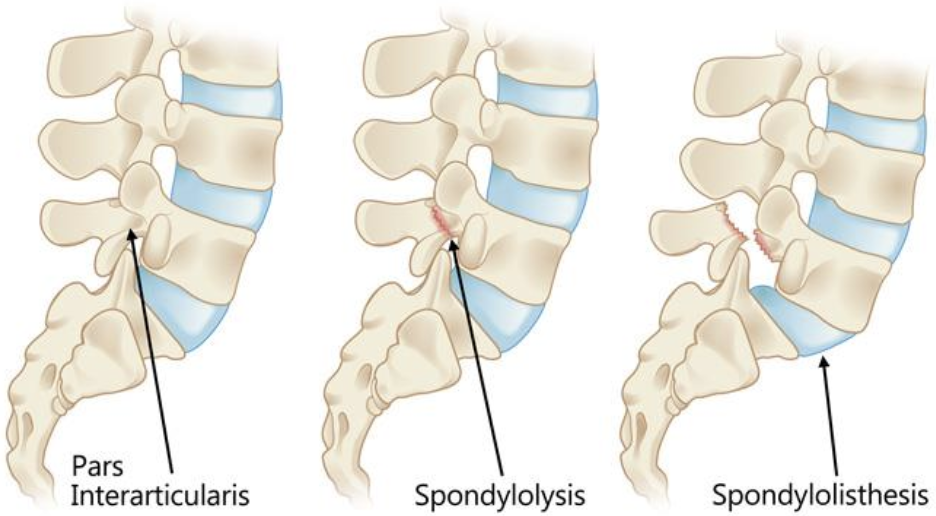
- Spondylolysis: Bony defect in pars interarticularis (usually L4 and L5)
- Spondylolisthesis: Displacement of vertebral body relative to inferior vertebral body
- Caused by repetitive microtrauma
- Most common causes of back pain in children >10yo; often in athletes engaged in sports w/ repetitive extension, flexion, and rotation
26.9.4.2 Signs & Symptoms
- Low back pain that worsens w/ activity, improves w/ rest
- Spondylolisthesis: May have radicular or cauda equina symptoms
26.9.4.3 Diagnosis
- Imaging:
- MRI is now study of choice
- XR: Poorly sensitive and do not assess acuity, but might be required prior to MRI
- Standing AP, lateral, oblique views: Visualize defect
- Flexion and extension views: Assess stability
26.9.4.4 Management
- Spondylolysis and low-grade spondylolisthesis → conservative (rest from sports for > 3 mos, NSAIDs, PT, back bracing)
- Higher-grade spondylolisthesis (or failure of conservative management) → consider surgical intervention
26.9.5 Spondyloarthropathies
26.9.5.1 Signs & Symptoms
- Insidious onset
- Often misdiagnosed w/ recurrent strains/sprains
- Pain worse at night, improves w/ activity
26.10 Head
26.10.1 Mild Traumatic Brain Injury (TBI) (Concussion)
Including Graduated Return-to-Sport Program
See ED chapter for Mild TBI section